Comment
Open access
Published: 09 July 2025
Increased testing is needed for Mpox in DR Congo to urgently curb disease spread
Prince Imani-Musimwa, Placide Mbala-Kingebeni, Stéphane Hans-Bateyi-Mustafa, Alfred Ombeni-Musimwa & Mija Ververs
Communications Medicine volume 5, Article number: 280 (2025)
The low testing rates of Mpox suspected cases remain a key factor in the continued spread of the disease in the Democratic Republic of Congo (DRC) and neighboring countries. Here, we highlight the causes, as well as the challenges and strategies needed to curb the spread of the current uncontrolled Mpox outbreak in the DRC.
...
Conclusion
The DRC is the epicenter of the Mpox outbreak, which remains a public health emergency of international concern. Despite numerous efforts to contain the current Mpox outbreak, the disease continues to spread in all provinces and neighboring countries. Following several years of war and given the precarious conditions, the country remains vulnerable to emerging diseases with limited resources for large-scale diagnostic capacities. The low testing rates in suspected Mpox patients show that many untested positive patients may be circulating in the community, as a source to continue the spread of the disease. With DRC’s position at the heart of Africa and its multiple crossings with its nine neighboring countries, the uncontrolled epidemic within the country will continue to pose a threat across Africa. Therefore, urgent action is needed to curb the spread of the disease in the DRC.
...
Announcement
Collapse
No announcement yet.
Discussion - Thoughts on a global outbreak of monkeypox
Collapse
X
-
Translation Google
DRC: First babies vaccinated against MPOX
June 26, 2025 at 12:25 PM
Pregnant women also took part in the international clinical study, which aims to protect expectant mothers against the virus.
Info By Belga
The first babies have been vaccinated against monkeypox (formerly known as monkeypox) in Boende, in the west-central Democratic Republic of Congo. " The end of the epidemic is not yet in sight ," the University of Antwerp (UAntwerpen) said in a statement Thursday.
Large-scale vaccination campaigns are currently hampered by the fact that the Pox vaccine is not approved for babies and pregnant women. The PregInPoxVac research project aims to address this. Pregnant women are at increased risk of complications from Pox and can transmit the virus.
In August 2024, the World Health Organization (WHO) declared a public health emergency of international concern, the highest-level health alert, regarding MPOX. In the DRC, the country hardest hit by the virus, more than 30,000 cases have been recorded, but this number could be much higher.
The PregInPoxVac project is being conducted jointly by the Universities of Antwerp and Kinshasa. This is the first study to evaluate the safety and immunogenicity (i.e., the ability of a substance to trigger an immune response) of the MVA-BN vaccine (Jynneos) in pregnant and postpartum women, as well as in infants. The vaccine is produced by the Danish biotechnology company Bavarian Nordic. Over the coming months, 215 pregnant women, 144 postpartum women, and 344 infants will participate in the study.
https://www.rtbf.be/article/rdc-les-premiers-bebes-ont-ete-vaccines-contre-le-mpox-11567763
Leave a comment:
-
Translation Google
MPOX is transmissible during pregnancy, reveals a Belgian-Congolese study
A new variant of MPOX can be transmitted from mother to child through the placenta during pregnancy, the Institute of Tropical Medicine (IMT) revealed on Thursday, following the publication of a study conducted in collaboration with the Congolese National Institute of Biomedical Research (INRB).
Belga
Agency
Published on 06/19/2025 at 6:18 p.m.
Transmission of the "Clade Ib" variant can lead to complications during pregnancy, such as miscarriage or stillbirth. MPOX has been linked to pregnancy complications in the past, but evidence of mother-to-child transmission remained limited prior to this study.
Three pregnant women infected during the recent spread of the virus in the Democratic Republic of Congo (DRC) were examined as part of this study. Research shows that MPOX can affect the fetus, like the rubella virus, the Zika virus, or chickenpox.
"The virus infected the fetuses through the placenta in all three women," explains Laurens Liesenborghs, Professor of Emerging Infectious Diseases at ITM. "The infection led to a miscarriage, a stillbirth, and a newborn with mpox. We diagnosed lesions on the faces and bodies of both the stillborn baby and the newborn."
Professor Placide Mbala-Kingebeni of the INRB stresses that urgent action is needed to protect pregnant women and stop infections in the DRC. "Vaccination and safe and effective treatments are essential in this regard," he explains.
The study was published in the medical journal The New England Journal of Medicine and was funded by the Flemish Fund for Scientific Research (FWO).
In August 2024, the World Health Organization (WHO) declared its highest-ever global alert for the mpox virus, also known as monkeypox. Last week, the WHO announced the extension of the health emergency.
 Un nouveau variant du mpox peut être transmis de la mère à l'enfant par le placenta pendant la grossesse, révèle jeudi l'Institut de médecine tropicale (IMT), après la publication d'une étude menée en collaboration avec l'Institut national de recherche biomédicale (INRB) congolais.
Un nouveau variant du mpox peut être transmis de la mère à l'enfant par le placenta pendant la grossesse, révèle jeudi l'Institut de médecine tropicale (IMT), après la publication d'une étude menée en collaboration avec l'Institut national de recherche biomédicale (INRB) congolais.
------------------------------------------
See also:
Three Cases of Vertical Transmission of Clade Ib Mpox Virus (The Lancet, Correspondence, June 18, 2025)
 Correspondence (https://www.nejm.org/browse/nejm-article-type/correspondence) Three Cases of Vertical Transmission of Clade Ib Mpox Virus Published June 18, 2025 N Engl J Med 2025;392:2385-2387 DOI: 10.1056/NEJMc2503347 VOL. 392 NO. 23 (https://www.nejm.org/toc/nejm/392/23) Copyright © 2025 (https://www.nejm.org/doi/full/10
Correspondence (https://www.nejm.org/browse/nejm-article-type/correspondence) Three Cases of Vertical Transmission of Clade Ib Mpox Virus Published June 18, 2025 N Engl J Med 2025;392:2385-2387 DOI: 10.1056/NEJMc2503347 VOL. 392 NO. 23 (https://www.nejm.org/toc/nejm/392/23) Copyright © 2025 (https://www.nejm.org/doi/full/10
Leave a comment:
-
Explosive mpox outbreak in Sierra Leone overwhelms health systems
Rapid transmission through sexual networks raises fears of wider spread in the region
2 Jun 20257:20 PM ET By Kai Kupferschmidt
...
Researchers from Sierra Leone reported on virological.org on 28 May that the virus belongs to clade IIb, a variant that circulated for several years in Nigeria before it suddenly caused a global outbreak in 2022, primarily among men who have sex with men (MSM). It continues to spread in MSM networks in many countries, but at a slower pace.
The variant is behaving very differently in Sierra Leone, however. Its explosive spread, combined with the fact that cases seem evenly split between men and women, initially led some scientists to believe the virus might have undergone changes that make it more transmissible without sexual contact. “The spread of Mpox in Sierra Leone is unlike anything we have ever seen,” Kristian Andersen, an evolutionary biologist at Scripps Research, wrote on Bluesky on 22 May. “This could be the next one.”
Other scientists point out that cases were roughly equally divided between men and women in recent outbreaks in the Democratic Republic of the Congo and its neighbor Burundi. Those were largely driven by sexual transmission. And like those countries, Sierra Leone is seeing many serious cases, including people who have lesions all over their bodies. Those outbreaks, however, were caused by a different variant of the virus, clade Ib. “We are still a bit puzzled by what is going on,” Boum says. “The situation [in Sierra Leone], while it is due to clade IIb, looks like a clade Ib in terms of transmission mode but also clinical features.” A team of 10 epidemiologists will be sent to the country to investigate, he says.
...
Leave a comment:
-
"Mpox is still increasing."
(Screenshot)
Weekly Special Press Briefing on Health Emergencies || April 3, 2025
https://www.youtube.com/watch?v=QJAL8-FIB3k
Leave a comment:
-
Translation Google
Mpox in the DRC: residents of a Kinshasa shanty town on the front line
Published: February 4, 2025 7:29am EST
Author
Yap Boom
Professor in the faculty of Medicine, Mbarara University of Science and Technology
...
Walking through the crowded streets of the Pakadjuma neighborhood in Kinshasa, capital of the Democratic Republic of Congo, I am struck by the vibrant atmosphere around me.
Children play happily in puddles, surrounded by piles of plastic bags and open sewage ditches. Shacks patched together with pieces of corrugated iron fill the city. Rumba music fills the air as young people party in open bars, waiting for grilled pork or chicken. Sex workers sit outside tin shacks in narrow alleys, hailing clients.
Nearby, a Médecins Sans Frontières sorting center is the only reminder that this shantytown is the epicentre of Kinshasa’s mpox outbreak. There are no posters, brochures or banners warning residents of the dangers of this viral disease that was declared a continental and global emergency in August last year.
At the clinic, patients suspected of having MPOX are referred to one of three specialized centers in the city. The most common symptoms are fever, headache, muscle aches, chills, exhaustion, swollen lymph nodes and lesions. With symptomatic care, most patients recover within 7 to 35 days, depending on the severity of the case.
As an epidemiologist co-leading the MPOX response for the Africa Centres for Disease Control and Prevention , I travelled to Pakadjuma to get a clearer picture of the situation on the ground.
MPOX is historically a rural disease in the DRC. This microcosm of Kinshasa highlights the complex challenges of managing the epidemic in a city.
Fighting on two fronts
With a population of over 17 million, Kinshasa is Africa's largest megacity . Pakadjuma is one of the city's many overcrowded neighborhoods where people live in extreme poverty.
Kinshasa, often called “Kin the Beautiful,” is facing a unique crisis in the fight against MPOX. Both strains of the virus, clade Ia and clade Ib, are circulating simultaneously in the city. This is the first time this has happened.
Clade Ia , which is transmitted primarily from animals to humans and then within households through touch, has been endemic in Africa for decades.
Clade Ib is a new strain that is primarily contracted through sexual contact. This is the strain that has spread rapidly across 21 African countries during the current outbreak in East and Central Africa.
This dual transmission makes the fight against MPOX even more complicated: how do we tackle a public health crisis rooted both in intimate human relationships and in structural inequalities such as living in crowded areas?
Although the strains are treated clinically similarly, their spread and transmission differ.
Clade Ia is primarily associated with zoonotic (animal-to-human) transmission in rural areas. Animal surveillance and community education are needed to control spillovers.
Clade Ib, which has higher human-to-human transmissibility, requires intensified contact tracing, vaccination and preventive measures in urban and peri-urban areas.
Adapting strategies to these differences is essential to contain the epidemic.
When Condoms Don't Work
Pakadjuma, in the northeast of the city, is known for its poverty and high crime rates. For many girls and young women, sex work is the only option available to survive.
One of the most pressing challenges in combating the virus in the region is curbing sexual transmission.
Unlike HIV, for which condoms can significantly reduce the risk of spread, smallpox poses a different problem: because the virus is transmitted by touch, there is no practical preventative measure for sexual transmission other than total abstinence.
Smallpox lesions develop in the groin, making any movement excruciating. For these sex workers, abstinence is not an option. It would mean losing their livelihood and the ability to feed their children.
As for their clients, who come from all over the city, they would have to change a key aspect of their lives for a disease they consider less deadly than Ebola . There is no easy answer to this dilemma.
Trace the spread
Contact tracing, a cornerstone of epidemic control, is another obstacle.
Identifying and tracing contacts of sex workers is complex. As a result, only a tiny fraction of MPOX cases are confirmed by laboratory testing.
On average, each mpox case has about twenty contacts, but it is virtually impossible to trace the clients of a highly confidential sex network.
In the absence of effective contact tracing, infected people remain in the community and often only seek treatment when their condition worsens. Discussions with Médecins Sans Frontières staff in the triage area show that suspected cases of COPD usually arrive at an advanced stage of the disease, when symptoms are clearly visible. Many patients first try other remedies, such as traditional healing methods, before seeking medical care.
Fortunately, Kinshasa has a strong network of laboratories led by the National Institute of Biomedical Research, and test results are available within 48 to 72 hours. This cutting-edge institute was created by Dr. Jean Jacques Muyembe , the microbiologist who discovered the Ebola virus.
During the first week of January 2025, there were 1,155 confirmed cases and 27 deaths in the city, according to the DRC Ministry of Health.
Even for those seeking treatment at specialist centres to combat the disease, navigating the chaotic and congested roads is a nightmare. The yellow minibuses - known locally as the "spirit of death" - are packed and it can take hours to reach their destination.
With the number of patients increasing, the city's MPOX treatment centres are overwhelmed.
The fight on all fronts
The fight against the MPOX epidemic in Kinshasa requires a multifaceted approach:
Vaccination: Widespread vaccination campaigns offer the best hope for controlling the outbreak in hotspots such as Pakadjuma, where contact tracing is nearly impossible. In these cases, the entire community must be vaccinated.
This could break chains of transmission while allowing those at risk, such as sex workers, to continue to work.
Prevention and control: Home-based care is essential, especially in informal settlements like Pakadjuma. Providing food and material support to patients and their families and encouraging isolation of infected relatives will help limit the spread of the disease.
These measures, however, require a new way of thinking as people try to survive day to day.
Engaging with the community: This is difficult because of the stigma surrounding the disease, but it must be at the heart of the response.
Amplify the message: Media, local leaders and trusted community members must be mobilized to get the message across effectively.
All this must be done without delay, otherwise the epidemic will be almost impossible to contain in this vast and sprawling city. The consequences would be disastrous.
Leave a comment:
-
WHO Director-General's opening remarks at the media briefing – 28 November 2024
28 November 2024
...
Now to mpox.
Last Friday, the Emergency Committee met and advised me that the outbreaks of mpox in Africa continue to represent a public health emergency of international concern. I accepted that advice.
Yesterday, the Emergency Committee issued updated temporary recommendations, adding some new recommendations, and extending or modifying others.
As we have said many times, we are not dealing with one outbreak of one virus, but several simultaneous and overlapping outbreaks of different strains, or clades of the virus, affecting different groups in different places.
So far this year, 20 countries in Africa have reported more than 14 thousand confirmed cases, including 55 deaths.
More than 75% of all confirmed cases and deaths in Africa this year have been in the Democratic Republic of the Congo, where the outbreak of clade 1b has now spread to six provinces, including the capital Kinshasa.
Clade 1b has also spread to four neighbouring countries:
In Burundi, more than 2 000 cases have been reported, largely in urban areas;
In Uganda, there are 649 cases and a fast-expanding epidemic, especially in the capital Kampala,
In Rwanda, 37 cases have been confirmed and in Kenya there are 19 cases;
And cases have also been reported in at least 8 other countries in Africa, the Americas and Europe.
WHO, Africa CDC and our partners are continuing to support countries to respond to these outbreaks and prevent further ones under our joint continental preparedness and response plan.
Together, we are strengthening the “five Cs” of outbreak response:
Coordination;
Collaborative surveillance and detection;
Community protection;
Care that is safe and scalable;
And countermeasures, including vaccines.
So far, six million vaccine doses have been pledged, of which 1.6 million are ready for distribution by the end of the year.
Almost 56 000 people have been vaccinated in 7 provinces of the DRC, and health officials there are preparing to administer a second dose, with vaccination starting in Kinshasa this week.
We still face many challenges to bring these outbreaks under control.
To meet them, we need stronger political commitment to scale up response activities;
We need fully resourced preparedness and response plans;
We need further contributions of medical countermeasures including diagnostics and vaccines;
And we need continued transparency and collaboration between affected countries and partners.
===
Leave a comment:
-
Stopping mpox: wild meat markets are a root cause and must be made safer
Published: November 5, 2024 7:40am EST
Authors
- Steven Lam
Postdoctoral Scientist, CGIAR System Organization 
- Delia Grace
Professor Food Safety Systems at the Natural Resources Institute (UK) and contributing scientist ILRI, International Livestock Research Institute
Steven Lam's work is part of the CGIAR One Health Initiative, which is supported by the CGIAR Trust Fund.
Delia Grace does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
...

A young hunter displays captured rats for sale, along with other bushmeat, in Cameroon, The country has also been hit by the current mpox outbreak. Nabila El Hadad/AFP via GettyImages
In many countries around the world, wild animals are sometimes killed for food, including monkeys, rats and squirrels.
Wild meat makes significant contributions to nutrition in Africa and to satisfying food preferences in Asia.
In Africa, the annual harvest of wild meat, estimated at between 1 million and 5 million metric tonnes, is substantial compared to the continent’s livestock production of about 14 million metric tonnes per year.
Public health researchers have long highlighted unhygienic wild meat practices as potentially harmful due to the risk of pathogens jumping from animals to humans, especially through close contact during hunting, processing or consuming undercooked meat.
This concern was particularly pronounced during the 2014 Ebola outbreak in the Democratic Republic of Congo. Ebola is known to jump from animals to humans, who are likely infected either by touching or consuming sick or dead infected forest animals, such as fruit bats.
Mpox is another zoonotic disease that is known to jump from animals to humans. More than 1,100 people have died of mpox in Africa, where some 48,000 cases have been recorded since January 2024 in 19 countries.
Strategies to beat the 2024 mpox outbreak have so far largely focused on preventing human-to-human transmission.
But we also need to go back to the root causes of disease, particularly where mpox is transmitted from animals to humans.
Applying lessons from food safety is key to solving this urgent public health concern.
‘Wet’ markets
Wild meat is often sold alongside other fresh foods in informal markets, also known as “wet” markets. These markets typically operate with little regulation and hygiene standards, which increases the risk of diseases.
We are public health researchers specialising in testing and evaluating solutions to zoonoses (when humans are infected with a disease by wild animals), antimicrobial resistance (when antibiotics are no longer effective) and food safety.
In a new paper, together with colleagues at CGIAR, a global partnership to address challenges of food systems, we look at promising solutions to address risks from wild meat.
Key to this is a One Health approach. One Health brings together public health experts, veterinarians, wildlife specialists and community leaders to develop comprehensive measures.
Three-legged stool
Our research has shown that food safety in hard-to-reach markets can be improved if, and only if, three key areas are addressed:
Capacity building: Capacity-building provides training and simple technologies to workers in food chains and consumers.
Food safety efforts in informal markets have traditionally focused on encouraging local communities to adopt safer practices.
Understanding how people see disease risk and what influences these perceptions is key.
In the Democratic Republic of Congo, for example, there was distrust of formal institutions and a rejection of government health messages linking Ebola to bushmeat.
In communities where people already recognise the risks associated with bushmeat, health messages could focus on practical, protective steps.
In places where scepticism exists, sharing evidence of health risks may be more successful.
Read more: Food safety policy neglects informal markets in developing countries - 3 ways this can change
Instead of pushing an anti-hunting agenda, a more helpful approach could involve providing ways to reduce the risk of disease transmission without completely discouraging hunting and consumption.
While this approach may not eliminate all risks, it is likely to be more effective than a campaign that fails to resonate with the community.
While having the right knowledge is important for encouraging change, there is also a need for incentives.
Motivation and incentives: Although food safety is a large concern for consumers worldwide, it often takes a back seat to affordability. For those who struggle to afford food, food safety is not a priority compared to cost.
Governments have frequently relied on bans and enforcement measures, including fines and inspections, as “negative incentives” for change.
Read more: Informal food markets: what it takes to make them safer
The Nigerian government prohibited the sale of bushmeat as a precaution to stop the spread of mpox in June 2022. However, these bans can have unintended consequences, such as driving bushmeat practices underground with worse hygiene practices.
Potentially more effective is to focus on economic, social, or moral gains.
Economic incentives might include describing the potential financial gains from attracting a larger customer base due to the credibility of safer meat.
Social incentives could involve earning the trust of community members.
Moral incentives could stem from the pride in ensuring that bushmeat is handled and sold in a way that reduces health risks.
Enabling policies and regulations: In some poorer communities, food safety laws are either nonexistent or not applicable to informal markets.
Recognising vendors who achieve notable improvements in food safety might inspire others to follow their lead.
Read more: Chickens from live poultry markets in Nigeria could be bad for your health - scientists explain why
Additionally, promoting alternative protein sources by providing access to affordable, nutritious food options and supporting sustainable agricultural practices can help to reduce reliance on bushmeat.
Looking forward
So, as countries plan their responses to mpox, three key considerations should be top of mind:- Firstly, it is important to recognise that bushmeat is a crucial part of many communities’ lives and contributes to their health and well-being.
- Secondly, responses should be developed with input from local communities which will increase the chances of success.
- Lastly, high-income countries should lead by not only sharing knowledge but also boosting funding for global health initiatives, as this can substantially reduce the risk of future outbreaks.
https://theconversation.com/stopping...e-safer-242120
Leave a comment:
-
Translation Google
In Kamituga, "sins" at the source of the mpox epidemic in the DRC
AFP , 09/30/2024 at 05:00 Modified on 09/30/2024 at 09:15
Gold panners, traders, prostitutes: at nightfall, hundreds of them crowd into the gloomy bars of Kamituga, a mining town in South Kivu, in the east of the Democratic Republic of Congo.
...
Kamituga, known for its gold mines, is the starting point of the epidemic which has been hitting the Democratic Republic of Congo (DRC) since September, according to health authorities
The deposits abandoned by Belgian companies in the 1990s attracted a host of artisanal miners and entrepreneurs of all kinds.
Today, there are some 300,000 inhabitants, double that number according to local estimates, walking the crowded streets of the city centre.
The buildings inherited from the colonial era have disappeared under a layer of dust and a jumble of makeshift buildings. Gold buying offices, gold panning equipment and, above all, nightclubs and bars for the "atmosphere" after a hard day's work in the mines.
...
"Some 20% of our patients are infected by sexual transmission and condoms do not protect," explains Dr. Dally Muamba Kambaji, from the NGO Alima.
Doctors at the local hospital were the first to face the resurgence of MPOX as early as September 2023.
"We noticed unusual skin lesions on the manager of a nightclub ," recalls Dr. James Wakilonga Zanguilwa.
"When we noticed that some free women in the same box started to develop similar lesions, we raised the alarm ," he continues.
The nightclub "Mambegeti" has since closed its doors but left its name to the disease. In Kamituga, prostitutes have been the main vector for the spread of "Mambegeti" , the local nickname for mpox.
...
Despite the pitiful state of National Road 2, which links Kamituga to the provincial capital, Bukavu, 180 kilometers away, the comings and goings of populations have spread the virus throughout the province of South Kivu, which has become the epicenter of the epidemic.
Leave a comment:
-

Krutika Kuppalli, MD FIDSA
@KrutikaKuppalli
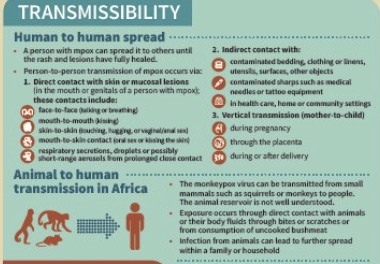
The @WHO has consistently stated that #Mpox transmission occurs through:
1. Direct contact - with skin/mucosal lesions - respiratory secretions, droplets or possibly short-range aerosols from prolonged close contact
2. Indirect contact - contaminated objects
3. Vertical transmission
4. Animal-to-human transmission
Leave a comment:
-
Krutika Kuppalli, MD FIDSA
@KrutikaKuppalli
·
12h
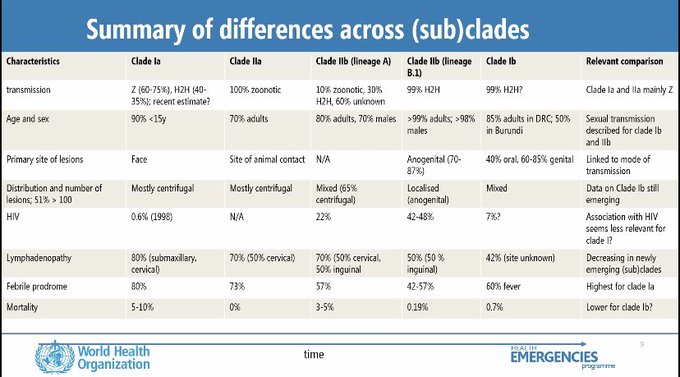
Impressive presentation by
@WHO
IMST at the
@rd_blueprint
meeting today! They shared a helpful summary of #mpox clades and subclades, while highlighting that there’s still a lot to learn.
Lorenzo Subissi and 2 others
Leave a comment:
-
WHO identifies droplets as 'minor' Mpox transmission risk
Hespress EN
Tuesday 27 August 2024 - 23:43
The World Health Organization (WHO) announced on Tuesday that droplets are considered a “minor” route of transmission for mpox, while emphasizing the need for additional research to fully understand how the virus spreads.
According to the WHO, mpox (formerly known as ‘monkeypox’) primarily spreads through close physical contact, including skin-to-skin, mouth-to-mouth, and mouth-to-skin interactions.
WHO spokesperson Margaret Harris explained during a press briefing that while it is possible for droplets to transmit the virus when an infected person speaks or breathes closely on another individual, this is a relatively minor source of transmission.
“if you’re talking closely to someone, breathing on them, physically close, face-to-face, there is a possibility” of viral spread,” Harris noted. However, she stressed that such cases are less common compared to other modes of transmission.
...
Leave a comment:
-
For the continent of Africa only:
ALL CLADES -
I attended the Africa CDC presser today. Dr. Kaseya showed a slide depicting 22,863 total mpox cases as of August 26, 2024 (3,641 confirmed and 19,222 suspected) and 622 deaths.
https://flutrackers.com/forum/forum/...gmt#post995850
Leave a comment:
-
Translation Google
DRC: A health worker, dogs, pigs and bats die from Mpox (By Miphy Buata, Debora Lusamba and Pierre Matadi)
August 26, 2024
Kinshasa, August 25, 2024 (ACP).- A health worker, dogs, pigs and bats have died from Mpox (Monkeypox) in the Democratic Republic of Congo, where the outbreak, declared an "emergency of international concern" by the World Health Organization (WHO) on August 14, has caused the death of nearly 600 people.
" This year, we have recorded 15 health workers infected with Mpox, including one death in Equateur ," said Dr. Cris Kacita, head of the Mpox operations section of the National Program to Combat Mpox and Viral Hemorrhagic Fevers (PNLMPOX-FHV).
In an internal document of the National Institute of Public Health (INSP), it is reported that in domestic fauna, 7 cases of dogs tested positive with 5 deaths were recorded; 5 pigs contaminated with 4 deaths. In wild fauna, 3 cases of bats were suspected.
Initially, scientists had indicated that monkeys and rodents were the main agents spreading the disease to humans.
With this announcement, it is worth noting that a new trend has taken up residence in the DRC, with dogs found in almost every household. It is not certain that all these domestic animals are followed by veterinarians.
The cumulative number of cases in 2024 rises to 18,077 suspected cases, including 4,843 confirmed cases, 615 deaths with a lethality of 3.4% and 3,456 recoveries, according to INSP statistics on Friday.
...
 Kinshasa, 25 août 2024 (ACP).- Un agent de santé, des chiens, des porcs et des chauves-souris sont décédés de Mpox (Variole de singe) en République démocratique du Congo, où l'épidémie, déclarée le 14 août « urgence de portée internationale » par l'Organisation mondiale de la Santé (OMS), a causé la…
Kinshasa, 25 août 2024 (ACP).- Un agent de santé, des chiens, des porcs et des chauves-souris sont décédés de Mpox (Variole de singe) en République démocratique du Congo, où l'épidémie, déclarée le 14 août « urgence de portée internationale » par l'Organisation mondiale de la Santé (OMS), a causé la…
Leave a comment:
-
Argentina Health Officials Rule Out Suspected Case of Mpox on Grains Ship
By Reuters
|
Aug. 21, 2024, at 11:54 a.m.
BUENOS AIRES (Reuters) -Health officials in Argentina said on Wednesday that a test to determine if a crew member on a quarantined grains cargo ship was infected with the mpox virus had come back negative, according to a statement from the health ministry.
The crew member, an Indian national who had developed cyst-like skin lesions on his chest and face, was working on the ship that was traveling along a key commodities route near the inland river port city of Rosario.
Authorities had quarantined the ship in the Parana River as a precaution.
In its statement, the health ministry said the individual tested negative for mpox, but positive for chicken pox.
Leave a comment:



Leave a comment: