Updated Interim Recommendations for Worker Protection and Use of Personal Protective Equipment (PPE) to Reduce Exposure to Novel Influenza A Viruses Associated with Disease in Humans
Español | Other Languages
Print
Updated April 26, 2024
Summary of changes
Take steps to reduce your risk of infection with avian influenza A viruses associated with severe disease when working with animals or materials, including raw milk, confirmed infected or potentially infected with these novel influenza A viruses. Examples of people working with or exposed to animals include:
Avoid unprotected direct or close physical contact with:
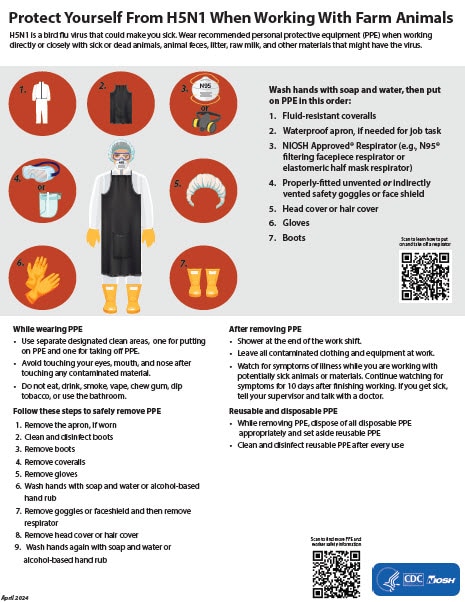
Protect Yourself From H5N1 When Working With Farm Animals [2 MB, 1 page]
Spanish [1.7 MB, 1 page]
If you must work in or enter any not yet disinfected buildings where these materials or sick or dead cattle or other animals confirmed infected or potentially infected are or were present, wear appropriate personal protective equipment (PPE) in addition to the PPE you might be using for your normal duties (e.g., waterproof apron, hearing protection, etc.). Appropriate PPE depends on the hazards present and a site-specific risk assessment. If you have questions on the type of PPE to use or how to fit it properly, ask your supervisor.
Recommended PPE to protect against novel influenza A viruses includes:
While wearing PPE
Note: Take off PPE by touching the least contaminated part of the PPE.
*Any change to the order of removing PPE should consider that the aim of the chosen sequence should be to minimize any contaminant transfer from potential contaminated protective clothing and equipment to the person’s skin or regular clothing.
All PPE should be used in accordance with OSHA regulations found at 29 CFR part 1910, Subpart I (Personal Protective Equipment), including identifying appropriate PPE based on a site-specific risk assessment. Workers must be trained on and demonstrate an understanding of when to use PPE; what PPE is necessary; what it looks like when PPE is properly fitted; how to properly put on, use, take off, dispose of, and maintain PPE; and understand the limitations of PPE.
Respirator use should be in the context of a comprehensive respiratory protection program in accordance with the Occupational Safety and Health Administration (OSHA) Respiratory Protection standard (29 CFR 1910.134) and other applicable requirements. Staff who will need to wear respirators must be medically-cleared, trained, and fit-tested for respirator use. Detailed information on respiratory protection programs, including fit testing procedures, can be accessed at OSHA’s Respiratory Protection eTool.
PPE training topics should include all the following:
For information on NIOSH Approved® respirators visit National Personal Protective Technology Laboratory. Important Considerations
It is important to wear the appropriate PPE for protection against dangerous hazards, including diseases, in the workplace. However, there are certain factors pertaining to the use of PPE of which employers and workers should be aware.
More Information
N95® and NIOSH Approved® are certification marks of the U.S. Department of Health and Human Services (HHS) registered in the United States and several international jurisdictions.
[i] Preferably, fluid-resistant coveralls should be made of material that passes:
[ii] Preferably, safety goggles should conform to ANSI Z87.1 that is marked at least Z87 D3
[iii] Preferably, gloves should conform to ASTM D3578 (latex rubber examination gloves), ASTM D5250 (vinyl examination gloves), ASTM D6319 (nitrile rubber examination gloves), or ASTM D6977 (chloroprene examination gloves). If thicker gloves are required, rubber gloves should be waterproof and exclude linings. If latex allergies are present, avoid latex. These gloves could be worn underneath the exterior principal glove (e.g., gloves for cold protection, manual shoveling) for protection against direct skin exposure if the outer glove is physically compromised.
Last Reviewed: April 26, 2024
Español | Other Languages
Updated April 26, 2024
Summary of changes
- This updated guidance identifies select occupational groups that may be at increased risk of exposure to novel influenza A viruses. Specific recommendations for these groups may be updated as CDC learns more during this evolving situation.
- Persons in these occupational groups should consult with their supervisor or their employer’s worker safety team to determine how best to apply these recommendations.
Take steps to reduce your risk of infection with avian influenza A viruses associated with severe disease when working with animals or materials, including raw milk, confirmed infected or potentially infected with these novel influenza A viruses. Examples of people working with or exposed to animals include:
- Poultry and livestock farmers and workers
- Backyard bird flock owners
- Veterinarians and veterinary staff
- Animal health responders
- Public health responders
- Slaughterhouse workers performing certain tasks on lactating dairy cattle including:
- Unloading or handling live lactating dairy cattle for slaughter, including workers in holding pens and involved with antemortem inspection
- Postmortem processes including the post-mortem inspection and handling and transporting viscera
- Removing and transporting udders from dairy cattle for further processing or rendering
Avoid unprotected direct or close physical contact with:
- Sick birds, livestock, or other animals
- Carcasses of birds, livestock, or other animals that have died from unknown causes
- Raw milk
- Viscera and udders from lactating dairy cattle
- Feces or litter
- Surfaces and water (e.g., ponds, waterers, buckets, pans, troughs) on farms with potentially infected animals that might be contaminated with animal waste
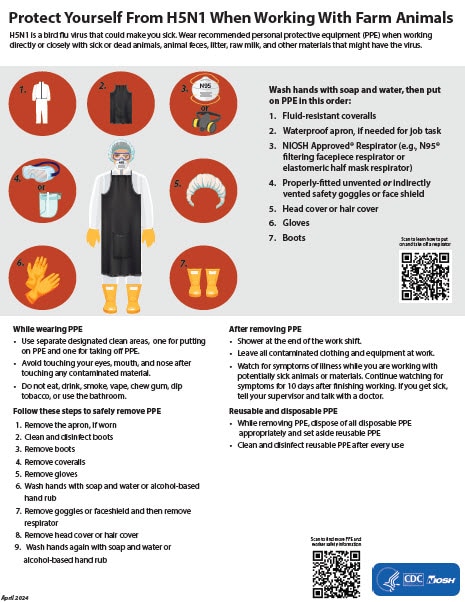
Protect Yourself From H5N1 When Working With Farm Animals [2 MB, 1 page]
Spanish [1.7 MB, 1 page]
If you must work in or enter any not yet disinfected buildings where these materials or sick or dead cattle or other animals confirmed infected or potentially infected are or were present, wear appropriate personal protective equipment (PPE) in addition to the PPE you might be using for your normal duties (e.g., waterproof apron, hearing protection, etc.). Appropriate PPE depends on the hazards present and a site-specific risk assessment. If you have questions on the type of PPE to use or how to fit it properly, ask your supervisor.
Recommended PPE to protect against novel influenza A viruses includes:
- Disposable or non-disposable fluid-resistant[i] coveralls, and depending on task(s), add disposable or non-disposable waterproof apron
- Any NIOSH Approved® particulate respirator (e.g., N95®or greater filtering facepiece respirator, elastomeric half mask respirator with a minimum of N95 filters)
- Properly-fitted unvented or indirectly vented safety goggles[ii] or a faceshield if there is risk of liquid splashing onto the respirator
- Rubber boots or rubber boot covers with sealed seams that can be sanitized or disposable boot covers for tasks taking a short amount of time
- Disposable or non-disposable head cover or hair cover
- Disposable or non-disposable gloves [iii]
While wearing PPE
- Avoid touching yourself above your chest, especially your eyes, mouth, or nose, after touching any contaminated material
- Do not eat, drink, smoke, vape, chew gum, dip tobacco, or use the bathroom
- Use separate designated clean areas, one for putting on PPE and another for taking it off
- Put PPE on in this order and in a clean environment avoiding contamination:
- Wash hands with soap and water
- Fluid-resistant coveralls
- Waterproof apron, if needed
- NIOSH Approved® respirator
- Properly-fitted, unvented or indirectly vented safety goggles or faceshield
- Head cover or hair cover
- Gloves
- Boots or boot covers
- Remove PPE in this order* making sure to dispose of all disposable PPE appropriately and to set aside all reusable PPE for cleaning after each use:
- Remove apron, if worn
- Clean and disinfect boots or boot covers
- Remove boots or boot covers
- Remove coveralls
- Remove gloves
- Wash your hands with soap and water or, if soap and water are not available, use an alcohol-based hand rub
- Remove goggles or faceshield
- Remove respirator
- Remove headcover or hair cover
- Wash your hands again with soap and water or, if soap and water are not available, use an alcohol-based hand rub
Note: Take off PPE by touching the least contaminated part of the PPE.
*Any change to the order of removing PPE should consider that the aim of the chosen sequence should be to minimize any contaminant transfer from potential contaminated protective clothing and equipment to the person’s skin or regular clothing.
- All reusable PPE (e.g., rubber boots, goggles, faceshield, waterproof apron, elastomeric half mask respirators) should be set aside, then cleaned and disinfected after every use. To clean and disinfect reusable PPE:
- Select an EPA-approved disinfectant that has label claims against influenza A viruses
- Follow manufacturer/label directions for safe use of disinfectants
- Clean reusable PPE until visible dirt is removed
- Disinfect reusable PPE according to the disinfectant and PPE manufacturer’s instructions
- If possible, shower at the end of the work shift and put on clean uncontaminated clothing. If there are no shower facilities on site, clean up as much as possible, put on uncontaminated clothing, leave straight from work to a shower, and put on clean clothing immediately afterward
- Leave all contaminated clothing and equipment at work
- Never take contaminated equipment or wear contaminated clothing outside the work area
- Follow laundering instructions:
- Wash laundry onsite with standard laundry detergent, and completely machine-dry at the highest temperature suitable for the material.
- Wear gloves and protective outerwear when handling soiled laundry.
- Use separate storage and transport bins for clean and dirty laundry.
- If there is no laundry on site, clothing to be laundered at home should be transported in a plastic bag, kept separate from household items, washed separately, and then thoroughly machine-dried at the highest temperature suitable for the material.
- Self-monitor for symptoms of illness every day while you are working with sick or potentially infected animals or animals known to be infected with novel influenza A viruses for 10 days after the last day of exposure to infected or potentially infected animals or contaminated materials. If you become sick during those 10 days, isolate yourself, tell your supervisor, and get instructions for seeking medical evaluation and treatment.
All PPE should be used in accordance with OSHA regulations found at 29 CFR part 1910, Subpart I (Personal Protective Equipment), including identifying appropriate PPE based on a site-specific risk assessment. Workers must be trained on and demonstrate an understanding of when to use PPE; what PPE is necessary; what it looks like when PPE is properly fitted; how to properly put on, use, take off, dispose of, and maintain PPE; and understand the limitations of PPE.
Respirator use should be in the context of a comprehensive respiratory protection program in accordance with the Occupational Safety and Health Administration (OSHA) Respiratory Protection standard (29 CFR 1910.134) and other applicable requirements. Staff who will need to wear respirators must be medically-cleared, trained, and fit-tested for respirator use. Detailed information on respiratory protection programs, including fit testing procedures, can be accessed at OSHA’s Respiratory Protection eTool.
PPE training topics should include all the following:
- Proper fit-testing, wearing, and use of respirators
- Safe removal of respirators
- Safe disposal of disposable respirators
- Cleaning and disinfection of, and recommended respirator cartridge change-out schedule for, reusable respirators
- Medical contraindications to respirator use
- Use of only NIOSH Approved® respirators
For information on NIOSH Approved® respirators visit National Personal Protective Technology Laboratory. Important Considerations
It is important to wear the appropriate PPE for protection against dangerous hazards, including diseases, in the workplace. However, there are certain factors pertaining to the use of PPE of which employers and workers should be aware.
- Respirators: For untrained persons who work with poultry and livestock, including children, it is important to remember that respirators are designed primarily to be used in workplaces by adults who are part of their employer’s respiratory protection program. The risks and benefits of using respirators without proper training and fit testing are uncertain. For a respirator to be most effective, it must form a seal to the face to keep particles from leaking around the edges. When not fit tested, a tight seal should be achieved following manufacturer’s instructions. Additionally, most respirators will be too big to form a proper seal for younger children’s faces, and some will be too big for people with smaller faces
- Heat illness: Employers and workers should be aware that wearing PPE and certain clothing ensembles can often increase your risk for heat-related illnesses. For more on this topic visit Limiting Heat Burden While Wearing PPE
- Vision: Try to prevent fogging of goggles and face masks. Employers and workers should be aware that under certain conditions, some PPE can alter or decrease your visual acuity and peripheral vision. Under these conditions, workers should pay closer attention to their surroundings for hazards such as animal movement; clothes snagging; cuts or punctures; and slips, trips, and falls
More Information
- Avian Influenza Current Situation
- Protecting Poultry Workers from Avian Influenza (Bird Flu)
- Avian Influenza – Control and Prevention | Occupational Safety and Health Administration (osha.gov)
N95® and NIOSH Approved® are certification marks of the U.S. Department of Health and Human Services (HHS) registered in the United States and several international jurisdictions.
[i] Preferably, fluid-resistant coveralls should be made of material that passes:
- AATCC 42 ≤ 1 g and AATCC 127 ≥ 50 cm H2O or EN 20811 ≥ 50 cm H2O; or
- ASTM F1670 (13.8 kPa); or
- ISO 16603 ≥ 3.5 kPA
[ii] Preferably, safety goggles should conform to ANSI Z87.1 that is marked at least Z87 D3
[iii] Preferably, gloves should conform to ASTM D3578 (latex rubber examination gloves), ASTM D5250 (vinyl examination gloves), ASTM D6319 (nitrile rubber examination gloves), or ASTM D6977 (chloroprene examination gloves). If thicker gloves are required, rubber gloves should be waterproof and exclude linings. If latex allergies are present, avoid latex. These gloves could be worn underneath the exterior principal glove (e.g., gloves for cold protection, manual shoveling) for protection against direct skin exposure if the outer glove is physically compromised.
Last Reviewed: April 26, 2024




Comment