Denmark SSI: Marked Increase In Parrot Fever Cases Over the Past 60 Days
#17,933
Psittacosis - often called parrot fever - is a rarely reported, atypical bacterial pneumonia caused by Chlamydia psittaci. The CDC cites an average of 10 cases of Psittacosis reported each year in the US, although many others may go undiagnosed.
The CDC also reports:
Since 1988, there has been a decline in reported psittacosis cases. This decline may be the result of improved diagnostic tests that distinguish Chlamydia psittaci from more common Chlamydia pneumoniae infections.
From time to time we see small outbreaks reported, usually in Asia (Japan Report 2 Fatal Cases of Parrot Fever (Psittacosis) In Pregnant Women) or in Europe (see 2007's To You, My Heart Cries Out Chlamydiaabout a small outbreak that occurred at a Bird lovers Society show in Weurt, Norway).
Until fairly recently, human infection has been solely attributed to direct or indirect contact with infected birds.
But in 2012, the journal Eurosurveillance carried a report called Psittacosis outbreak in Tayside, Scotland, December 2011 to February 2012, involving four family members and a health-care worker, which suggested human-to-human transmission.
The following year, in Sweden Reports Rare Outbreak Of Parrot Fever,we saw a credible report of human transmission of parrot fever, where a 75 year old man who died in Kronoberg appeared to have spread the infection to at least 8 close contacts, including healthcare personnel.
In 2014, the ECDC's Eurosurveillance Journal carried a follow up report called:
Eurosurveillance, Volume 19, Issue 42, 23 October 2014
Surveillance and outbreak reports
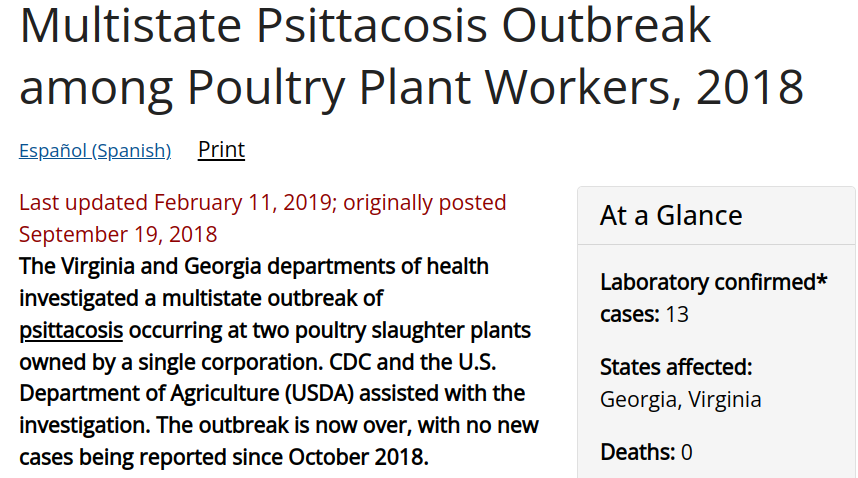
And in 2018 we saw another example, in PLoS Currents: A Psittacosis Outbreak Among Office Workers With Little Or No Bird Contact - UK. In 2022 the Lancet published a correspondence (see Gestational psittacosis: an emerging infection) that called:
`Human-to-human transmission of psittacosis is an emerging public health risk to medical workers and other close contacts, including pregnant women.'
While H-2-H transmission of C. psittaci now appears possible, contact with infected birds remains the primary suspected route of transmission.
Today Denmark's SSI is reporting an uptick in Psittacosis cases (n=23 since December 20th), which is roughly as many as they see in an average year. Notably, most of these cases report no known contact with birds.
This report mentions other European countries reporting cases (see Health alert after parrot fever infects humans in Sweden). I'll have a bit more after the (translated) statement.
Several cases of parrot disease/ornithosis in Denmark
During the past two months, there have been more cases of parrot disease in Denmark than usual. The disease spreads from birds to humans. SSI therefore encourages doctors to be aware of the disease.
(Continue . . . )
Fourteen years ago, in How Parrot Fever Changed Public Health In America, I wrote about the 1929 Parrot Fever epidemic which briefly revived fears of a new pandemic 10 years after the Spanish Flu.
While overblown by the newspapers eager for something other than the stock market crash to focus on, at least 169 people were diagnosed with the illness across several states, and 33 died.
Among the dead were 3 members of the public health team investigating the outbreak (Dr. Daniel S. Hatfield and Dr. William Stokes of the Baltimore Health Department, and Henry (Shorty) Anderson of the Hygienic Lab).
The outbreak was finally quashed, but out of it (and concerns over the recent rise in flu) came funding from Congress for a new, better staffed and equipped laboratory to replace the old Hygienic Lab.
They also gave it a new name: The National Institute of Health.
Today, treatment of Psittacosis is much easier than it was in 1930, as it generally responds well to Tetracyclines.
#17,933
Psittacosis - often called parrot fever - is a rarely reported, atypical bacterial pneumonia caused by Chlamydia psittaci. The CDC cites an average of 10 cases of Psittacosis reported each year in the US, although many others may go undiagnosed.
The CDC also reports:
Since 1988, there has been a decline in reported psittacosis cases. This decline may be the result of improved diagnostic tests that distinguish Chlamydia psittaci from more common Chlamydia pneumoniae infections.
From time to time we see small outbreaks reported, usually in Asia (Japan Report 2 Fatal Cases of Parrot Fever (Psittacosis) In Pregnant Women) or in Europe (see 2007's To You, My Heart Cries Out Chlamydiaabout a small outbreak that occurred at a Bird lovers Society show in Weurt, Norway).
Until fairly recently, human infection has been solely attributed to direct or indirect contact with infected birds.
But in 2012, the journal Eurosurveillance carried a report called Psittacosis outbreak in Tayside, Scotland, December 2011 to February 2012, involving four family members and a health-care worker, which suggested human-to-human transmission.
The following year, in Sweden Reports Rare Outbreak Of Parrot Fever,we saw a credible report of human transmission of parrot fever, where a 75 year old man who died in Kronoberg appeared to have spread the infection to at least 8 close contacts, including healthcare personnel.
In 2014, the ECDC's Eurosurveillance Journal carried a follow up report called:
Eurosurveillance, Volume 19, Issue 42, 23 October 2014
Surveillance and outbreak reports
Proven transmission of Chlamydia psittaci between humans has been described on only one occasion previously. We describe an outbreak which occurred in Sweden in early 2013, where the epidemiological and serological investigation suggests that one patient, severely ill with psittacosis after exposure to wild bird droppings, transmitted the disease to ten others: Two family members, one hospital roommate and seven hospital caregivers. Three cases also provided respiratory samples that could be analysed by PCR. All the obtained C. psittaci sequences were indistinguishable and clustered within genotype A.
The finding has implications for the management of severely ill patients with atypical pneumonia, because these patients may be more contagious than was previously thought. In order to prevent nosocomial person-to-person transmission of C. psittaci, stricter hygiene measures may need to be applied.
And in 2018 we saw another example, in PLoS Currents: A Psittacosis Outbreak Among Office Workers With Little Or No Bird Contact - UK. In 2022 the Lancet published a correspondence (see Gestational psittacosis: an emerging infection) that called:
`Human-to-human transmission of psittacosis is an emerging public health risk to medical workers and other close contacts, including pregnant women.'
While H-2-H transmission of C. psittaci now appears possible, contact with infected birds remains the primary suspected route of transmission.
Today Denmark's SSI is reporting an uptick in Psittacosis cases (n=23 since December 20th), which is roughly as many as they see in an average year. Notably, most of these cases report no known contact with birds.
This report mentions other European countries reporting cases (see Health alert after parrot fever infects humans in Sweden). I'll have a bit more after the (translated) statement.
Several cases of parrot disease/ornithosis in Denmark
During the past two months, there have been more cases of parrot disease in Denmark than usual. The disease spreads from birds to humans. SSI therefore encourages doctors to be aware of the disease.
Last edited on March 1, 2024
Since 20 December 2023, 23 cases of parrot disease in humans have been detected in Denmark. Normally we register around 15-30 cases in a whole year.
"We are currently experiencing more cases than usual, and we hear the same message from other colleagues around Europe. That is why we ask doctors in practice and in hospitals to pay particular attention to the disease," says senior researcher Søren Uldum from the Statens Serum Institut.
Parrot disease is also called ornithosis (bird disease), as it is not only parrots that can infect humans. It is a bacterial respiratory infection caused by the bacterium Chlamydia psittaci. The bacterium can be transmitted from infected birds to humans through close contact, but can also be transmitted by inhaling atomized particles from feathers or excrement. People are most often infected from domestic birds or various hobby birds such as ring pigeons. Most of the patients infected this winter report no or unknown contact with birds, while some report having fed birds at bird trays or automatic feeders.
"We suspect that the main cause of the infection must be found among wild birds, and we have several measures underway to examine samples from wild birds in an attempt to clarify this."Søren Uldum, senior researcher, Statens Serum Institut.
Parrot disease is in most cases a mild disease, and most often presents with flu-like symptoms such as fever, muscle aches and headaches. In some people, it can develop into a severe pneumonia affecting several organs. The disease can be treated with antibiotics.
In general, you should not be afraid to feed the birds in the garden, but you can follow these tips:
Since 20 December 2023, 23 cases of parrot disease in humans have been detected in Denmark. Normally we register around 15-30 cases in a whole year.
"We are currently experiencing more cases than usual, and we hear the same message from other colleagues around Europe. That is why we ask doctors in practice and in hospitals to pay particular attention to the disease," says senior researcher Søren Uldum from the Statens Serum Institut.
Parrot disease is also called ornithosis (bird disease), as it is not only parrots that can infect humans. It is a bacterial respiratory infection caused by the bacterium Chlamydia psittaci. The bacterium can be transmitted from infected birds to humans through close contact, but can also be transmitted by inhaling atomized particles from feathers or excrement. People are most often infected from domestic birds or various hobby birds such as ring pigeons. Most of the patients infected this winter report no or unknown contact with birds, while some report having fed birds at bird trays or automatic feeders.
"We suspect that the main cause of the infection must be found among wild birds, and we have several measures underway to examine samples from wild birds in an attempt to clarify this."Søren Uldum, senior researcher, Statens Serum Institut.
Parrot disease is in most cases a mild disease, and most often presents with flu-like symptoms such as fever, muscle aches and headaches. In some people, it can develop into a severe pneumonia affecting several organs. The disease can be treated with antibiotics.
In general, you should not be afraid to feed the birds in the garden, but you can follow these tips:
- Do not touch dead birds. If you find several dead or sick wild birds within a small area, it can be reported to the Danish Veterinary and Food Administration, primarily because of the risk of bird flu.
- If you have to clean (sweep/rake) where there have been birds at feeding places, in outbuildings and the like, you should wet the surface beforehand so that it does not create dust.
- If you find dead or sick birds in the garden, you must stop feeding them.
- You must then scald the places where there has been feed and water.
- Wash hands after contact with wild birds, feeding area or droppings.
(Continue . . . )
Fourteen years ago, in How Parrot Fever Changed Public Health In America, I wrote about the 1929 Parrot Fever epidemic which briefly revived fears of a new pandemic 10 years after the Spanish Flu.
While overblown by the newspapers eager for something other than the stock market crash to focus on, at least 169 people were diagnosed with the illness across several states, and 33 died.
Among the dead were 3 members of the public health team investigating the outbreak (Dr. Daniel S. Hatfield and Dr. William Stokes of the Baltimore Health Department, and Henry (Shorty) Anderson of the Hygienic Lab).
The outbreak was finally quashed, but out of it (and concerns over the recent rise in flu) came funding from Congress for a new, better staffed and equipped laboratory to replace the old Hygienic Lab.
They also gave it a new name: The National Institute of Health.
Today, treatment of Psittacosis is much easier than it was in 1930, as it generally responds well to Tetracyclines.



Comment