Re: Canada - H5N1 death in Alberta after travel from China - died from meningoencephalitis
[Source: ProMedMail.org, full page: (LINK). Edited.]
Published Date: 2014-01-12 10:23:15 / Subject: PRO/AH/EDR> Avian influenza, human (13): Canada ex China (BJ) H5N1, fatal, case report / Archive Number: 20140112.2167282
AVIAN INFLUENZA, HUMAN (13): CANADA ex CHINA (BEIJING), H5N1, FATAL, CASE REPORT
A ProMED-mail post http://www.promedmail.org / ProMED-mail is a program of the International Society for Infectious Diseases http://www.isid.org
Date: Sat 11 Jan 2014 / From: Kevin Fonseca <kevin.fonseca@albertahealthservices.ca> [edited]
_____
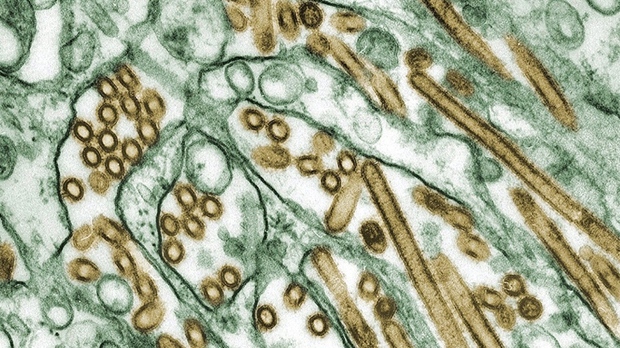
Avian influenza A(H5N1) was detected in the respiratory samples and CSF [cerebrospinal fluid] of a young adult, who died from the infection 7 days after returning from a vacation in Beijing, China accompanied by a family member.
The individual left Canada for China on 6 Dec 2013 and was exclusively in Beijing, in urban locations. There was no contact reported with live poultry, no visits to wet markets, or handling of fresh poultry. Work is ongoing to obtain a detailed account of activities during the trip.
During the return flight on 27 Dec 2013, the individual experienced symptoms of malaise, chest pain, and fever and presented to the local Emergency Department on 28 Dec 2013. The complete blood count (CBC) showed a total white blood count (WBC) of 12.6 x 10 to the power of 9/L (reference range 4.0 - 10.0 x10 to the power of 9/L) with raised neutrophils (11.1 x 10 to the power of 9/L) and low lymphocytes (0.8 x 10 to the power of 9/L). A chest X-ray and CT scan revealed a right apical infiltrate. A diagnosis of pneumonia was made; the patient was prescribed levofloxacin and discharged home.
The individual returned to the same Emergency Department on 1 Jan 2014, now with worsening pleuritic [inflammation of the membrane surrounding the lung] chest pains and shortness of breath, a mild headache, exacerbated by head movement, right upper quadrant and epigastric pain, nausea and vomiting with no diarrhea. A chest X-ray showed a multi-lobar pneumonia, with moderate effusion, reflecting significant progression when compared with the X-ray from the 1st ED visit. A thoracentesis [a procedure to remove excess fluid in the space between the lungs and the chest wall], performed while in the ED, revealed a dark amber cloudy fluid that was sterile in bacterial culture. The CBC again showed a WBC count of 10.2 x 10 to the power of 9/L, neutrophil count of 9.5 x 10 to the power of 9/L, platelet count within the normal range, normal ALT, slightly elevated AST at 46 U/L (reference range 7 - 40 U/L) and LDH at 288 U/L (reference range 100 - 225 U/L).
Admission to a general medicine ward for investigation was facilitated, and treatment was initiated with intravenous piperacillin-tazobactam. On 2 Jan 2014, the individual reported visual changes and ongoing headache, and, coupled with increasing oxygen requirements, was admitted to the ICU for intubation and ventilation. In the early morning of 3 Jan 2014, the individual developed a sudden episode of tachycardia and severe hypertension followed by hypotension requiring inotropic support. At this point, pupils were dilated, and there was no response to pain.
A CT brain scan suggested diffuse encephalitis and intracranial hypertension. The neurological examination was consistent with brain death. An MRI/MRA showed significant generalized edema, evidence of meningitis and ventriculitis [inflammation of the ventricles in the brain] and significant reduction in cerebral blood flow.
A lumbar puncture was performed after brain death determination and prior to removal of ventilatory and inotropic support. The attending physician felt that, while unlikely, avian influenza was possible given the travel history and neurological symptoms, and contacted the local Medical Officer of Health on 3 Jan 2014 to report to public health. Contact tracing of family and hospital contacts was initiated as a precaution, given the severity of the illness and its rapid progression.
Laboratory investigations:
Blood cultures were negative as were cultures of the broncho-alveolar lavage (BAL) fluids for a range of bacterial pathogens. Nasopharyngeal swabs and BAL were sent to the Provincial Laboratory for complementary viral investigations for influenza and other respiratory viral agents, and CSF for the herpesvirus group, enterovirus and parechoviruses.
Screening for influenza A and B and other respiratory viruses was performed on the respiratory samples (2 nasopharyngeal swabs and a BAL) through a combination of a direct fluorescent antigen (DFA) test (D3 Ultra DFA Influenza A/B reagent, Diagnostic Hybrids, Ohio), real time singleplex Taqman assays to influenza A and B assays targeting the matrix (M) gene of influenza A and NS1 gene of influenza B (1), and Luminex Respiratory Viral panel (Luminex, Ontario).
The swabs were negative by the DFA, however all these samples were positive for influenza A, with good Ct values in the Taqman assay, and were immediately subtyped, using real time assays to A(H1N1) pdm09 and seasonal H3 (2,3). Negative subtyping results were obtained on 2 independent runs, and when viewed in conjunction with recent travel history, strongly pointed to the possibility that this strain could be one of the avian subtypes known to occasionally infect humans. To investigate this possibility, a combination of real time and gel-based assays were performed to target the following genes H5, H7 and N9, on the viral RNA from the BAL, which had the highest titre of virus. Additionally, the M (matrix), NA (neuraminidase) and HA (haemagglutinin) genes were amplified and sequenced.
A compilation of the results from all these assays indicated that this strain was an influenza A(H5N1) subtype. Supplementary testing performed at the National Microbiology Reference Laboratory, Winnipeg, confirmed our findings that this was an avian influenza A (H5N1) virus.
Sequence data of the HA and NA genes from both laboratories showed the following.
From the HA sequence this virus;
The NA sequence shows genotypic sensitivity to oseltamivir (Tamiflu) based upon the histidine residue at position 275. This genotypic susceptibility result was considered to be helpful information as chemoprophylaxis with oseltamivir had been prescribed for close contacts of the individual.
Of interest is that the respiratory samples tested negative for influenza A in the Luminex Respiratory Viral panel but identified a human coronavirus 229E in the nasopharyngeal swabs, but not from the BAL. The negative influenza A results from this commercial assay were in contrast to the positive results obtained from the in-house Taqman assays.
The CSF collected also tested positive for influenza A and subtyped as H5.
An autopsy was not done due to concerns regarding the risk of virus transmission.
This case identifies a number of key issues, the 1st being the rapid onset and tragic death of a young, healthy traveler due to an avian influenza A(H5N1) infection. The index of suspicion was low as travel was to an area in China where there have been no recent reports of the circulation of this virus, and coupled with no obvious exposure to poultry, the diagnostic work-up and consideration for A(H5N1) infection was very low.
The clinical course, detection of the virus in the CSF, and results of imaging studies are consistent with an infection of the brain. A review of the literature indicates that such events are uncommon in humans, although animal models show that this virus is neurotropic and neuroinvasive (4,5).
From a laboratory diagnosis aspect, this case shows the value of having screening assays, in-house or commercial, known to be capable of identifying all influenza subtypes. Often, the proprietary information of the target and detection sites of commercial assays makes it difficult to know if non-seasonal subtypes can be detected (6). In this case, the discrepant results between our in-house screening Taqman assays and the Luminex Respiratory Viral Panel were very helpful in indicating this strain was not a seasonal subtype.
The availability of advanced molecular tools at the Alberta Provincial Laboratory allowed us to suspect, within 24 hours of testing these samples, that this was an unusual strain. Such information was valuable in implementing appropriate communication processes to healthcare workers who cared for this patient and to regularly update the appropriate authorities.
Finally, this infection of a Canadian resident is the 1st case of influenza A(H5N1) occurring in North America.
References
Lead and corresponding authors
Additional authors in alphabetical order by organization and last name:
Acknowledgments
The named authors would like to acknowledge the timely, thorough and expert contributions made by local medical, nursing, public health, infection control, and health care professionals to this work and this publication. At the request of the family, to preserve confidentiality, additional contributing authors have agreed not to be named. We would also like to express particular thanks to the family for their kind cooperation in this difficult time for them.
--
Kevin Fonseca, PhD, D(ABMM) / Clinical Virologist, Provincial Laboratory of Public Health / Alberta Health Services / Canada kevin.fonseca@albertahealthservices.ca
[ProMED is grateful to Kevin Fonseca and colleagues for providing this authoritative information. This report provides many additional historical, clinical and laboratory details of the recent fatal case of H5N1 influenza in a Canadian traveler returned from Beijing. (Media reports have stated that the patient was a female healthcare worker originally from China, in her 20s.) Notable features include the absence of apparent contact with poultry (though investigation is ongoing), the presence of pneumonia progressing from the right apex to multiple lobes and pleural effusion, the presence of intracranial edema, and radiographic evidence of inflammation of the meninges. It does not appear that influenza was suspected early enough to institute timely antiviral therapy.
H5N1 influenza A virus was detected from respiratory samples and from cerebrospinal fluid by nucleic acid amplification methods. Sequence analysis confirmed the identity of the virus and is indicative of viral features including high-pathogenicity, absence of oseltamivir resistance mutations at position 275, and wild-type affinity for the avian sialic acid receptor. - Mod.LM
A HealthMap/ProMED-mail map can be accessed at: http://healthmap.org/r/1zaU.]
(?)
-
-------
[Source: ProMedMail.org, full page: (LINK). Edited.]
Published Date: 2014-01-12 10:23:15 / Subject: PRO/AH/EDR> Avian influenza, human (13): Canada ex China (BJ) H5N1, fatal, case report / Archive Number: 20140112.2167282
AVIAN INFLUENZA, HUMAN (13): CANADA ex CHINA (BEIJING), H5N1, FATAL, CASE REPORT
A ProMED-mail post http://www.promedmail.org / ProMED-mail is a program of the International Society for Infectious Diseases http://www.isid.org
Date: Sat 11 Jan 2014 / From: Kevin Fonseca <kevin.fonseca@albertahealthservices.ca> [edited]
_____
Avian influenza A(H5N1) was detected in the respiratory samples and CSF [cerebrospinal fluid] of a young adult, who died from the infection 7 days after returning from a vacation in Beijing, China accompanied by a family member.
The individual left Canada for China on 6 Dec 2013 and was exclusively in Beijing, in urban locations. There was no contact reported with live poultry, no visits to wet markets, or handling of fresh poultry. Work is ongoing to obtain a detailed account of activities during the trip.
During the return flight on 27 Dec 2013, the individual experienced symptoms of malaise, chest pain, and fever and presented to the local Emergency Department on 28 Dec 2013. The complete blood count (CBC) showed a total white blood count (WBC) of 12.6 x 10 to the power of 9/L (reference range 4.0 - 10.0 x10 to the power of 9/L) with raised neutrophils (11.1 x 10 to the power of 9/L) and low lymphocytes (0.8 x 10 to the power of 9/L). A chest X-ray and CT scan revealed a right apical infiltrate. A diagnosis of pneumonia was made; the patient was prescribed levofloxacin and discharged home.
The individual returned to the same Emergency Department on 1 Jan 2014, now with worsening pleuritic [inflammation of the membrane surrounding the lung] chest pains and shortness of breath, a mild headache, exacerbated by head movement, right upper quadrant and epigastric pain, nausea and vomiting with no diarrhea. A chest X-ray showed a multi-lobar pneumonia, with moderate effusion, reflecting significant progression when compared with the X-ray from the 1st ED visit. A thoracentesis [a procedure to remove excess fluid in the space between the lungs and the chest wall], performed while in the ED, revealed a dark amber cloudy fluid that was sterile in bacterial culture. The CBC again showed a WBC count of 10.2 x 10 to the power of 9/L, neutrophil count of 9.5 x 10 to the power of 9/L, platelet count within the normal range, normal ALT, slightly elevated AST at 46 U/L (reference range 7 - 40 U/L) and LDH at 288 U/L (reference range 100 - 225 U/L).
Admission to a general medicine ward for investigation was facilitated, and treatment was initiated with intravenous piperacillin-tazobactam. On 2 Jan 2014, the individual reported visual changes and ongoing headache, and, coupled with increasing oxygen requirements, was admitted to the ICU for intubation and ventilation. In the early morning of 3 Jan 2014, the individual developed a sudden episode of tachycardia and severe hypertension followed by hypotension requiring inotropic support. At this point, pupils were dilated, and there was no response to pain.
A CT brain scan suggested diffuse encephalitis and intracranial hypertension. The neurological examination was consistent with brain death. An MRI/MRA showed significant generalized edema, evidence of meningitis and ventriculitis [inflammation of the ventricles in the brain] and significant reduction in cerebral blood flow.
A lumbar puncture was performed after brain death determination and prior to removal of ventilatory and inotropic support. The attending physician felt that, while unlikely, avian influenza was possible given the travel history and neurological symptoms, and contacted the local Medical Officer of Health on 3 Jan 2014 to report to public health. Contact tracing of family and hospital contacts was initiated as a precaution, given the severity of the illness and its rapid progression.
Laboratory investigations:
Blood cultures were negative as were cultures of the broncho-alveolar lavage (BAL) fluids for a range of bacterial pathogens. Nasopharyngeal swabs and BAL were sent to the Provincial Laboratory for complementary viral investigations for influenza and other respiratory viral agents, and CSF for the herpesvirus group, enterovirus and parechoviruses.
Screening for influenza A and B and other respiratory viruses was performed on the respiratory samples (2 nasopharyngeal swabs and a BAL) through a combination of a direct fluorescent antigen (DFA) test (D3 Ultra DFA Influenza A/B reagent, Diagnostic Hybrids, Ohio), real time singleplex Taqman assays to influenza A and B assays targeting the matrix (M) gene of influenza A and NS1 gene of influenza B (1), and Luminex Respiratory Viral panel (Luminex, Ontario).
The swabs were negative by the DFA, however all these samples were positive for influenza A, with good Ct values in the Taqman assay, and were immediately subtyped, using real time assays to A(H1N1) pdm09 and seasonal H3 (2,3). Negative subtyping results were obtained on 2 independent runs, and when viewed in conjunction with recent travel history, strongly pointed to the possibility that this strain could be one of the avian subtypes known to occasionally infect humans. To investigate this possibility, a combination of real time and gel-based assays were performed to target the following genes H5, H7 and N9, on the viral RNA from the BAL, which had the highest titre of virus. Additionally, the M (matrix), NA (neuraminidase) and HA (haemagglutinin) genes were amplified and sequenced.
A compilation of the results from all these assays indicated that this strain was an influenza A(H5N1) subtype. Supplementary testing performed at the National Microbiology Reference Laboratory, Winnipeg, confirmed our findings that this was an avian influenza A (H5N1) virus.
Sequence data of the HA and NA genes from both laboratories showed the following.
From the HA sequence this virus;
- (a) belongs to clade 2.3.2.1,
- (b) is a highly pathogenic influenza A(H5), based upon the presence of multiple basic amino-acid residues occurring at the cleavage site,
- (c) has a wild-type receptor binding site, consistent with preferential affinity for the avian alpha-2-3 sialic-acid receptor.
The NA sequence shows genotypic sensitivity to oseltamivir (Tamiflu) based upon the histidine residue at position 275. This genotypic susceptibility result was considered to be helpful information as chemoprophylaxis with oseltamivir had been prescribed for close contacts of the individual.
Of interest is that the respiratory samples tested negative for influenza A in the Luminex Respiratory Viral panel but identified a human coronavirus 229E in the nasopharyngeal swabs, but not from the BAL. The negative influenza A results from this commercial assay were in contrast to the positive results obtained from the in-house Taqman assays.
The CSF collected also tested positive for influenza A and subtyped as H5.
An autopsy was not done due to concerns regarding the risk of virus transmission.
This case identifies a number of key issues, the 1st being the rapid onset and tragic death of a young, healthy traveler due to an avian influenza A(H5N1) infection. The index of suspicion was low as travel was to an area in China where there have been no recent reports of the circulation of this virus, and coupled with no obvious exposure to poultry, the diagnostic work-up and consideration for A(H5N1) infection was very low.
The clinical course, detection of the virus in the CSF, and results of imaging studies are consistent with an infection of the brain. A review of the literature indicates that such events are uncommon in humans, although animal models show that this virus is neurotropic and neuroinvasive (4,5).
From a laboratory diagnosis aspect, this case shows the value of having screening assays, in-house or commercial, known to be capable of identifying all influenza subtypes. Often, the proprietary information of the target and detection sites of commercial assays makes it difficult to know if non-seasonal subtypes can be detected (6). In this case, the discrepant results between our in-house screening Taqman assays and the Luminex Respiratory Viral Panel were very helpful in indicating this strain was not a seasonal subtype.
The availability of advanced molecular tools at the Alberta Provincial Laboratory allowed us to suspect, within 24 hours of testing these samples, that this was an unusual strain. Such information was valuable in implementing appropriate communication processes to healthcare workers who cared for this patient and to regularly update the appropriate authorities.
Finally, this infection of a Canadian resident is the 1st case of influenza A(H5N1) occurring in North America.
With the rapidity of travel between countries and continents and the globalization of many cultures, this will likely not be the last case to occur in North America.
- Swine Influenza CDC Realtime RTPCR (rRTPCR) Protocol for Detection and Characterization of Swine Influenza (version 2009). CDC REF. #I-007-05 Page 1 of 8 Version 2009.
- CDC Realtime RTPCR (rRTPCR) Protocol for Detection and Characterization of Influenza (version 2007).
- Pabbaraju K, S Wong, AW Wong, GD Appleyard, et al. Design and Validation of Real-Time Reverse Transcription-PCR Assays for Detection of Pandemic (H1N1) 2009 Virus. J Clin Microbiol 2009;47(11):3454-60.
- Gambatto A, SM Barratt-Boyes, MD de Jong and Y Kawaoka. Human infections with highly pathogenic H5N1 influenza virus. Lancet 2007;371:1464-75.
- Lipatov AS, A Krauss, Y Guan, M Peiris et al. Neurovirulence in mice of H5N1 influenza virus genotypes isolated from Hong Kong poultry in 2001. J. Virol 2003;77(6):3816-3823.
- Hatchette TF, SJ Drews, N Bastien, Y. Li et al. Detection of Influenza H7N9 virus: all molecular tests are not equal. J Clin Microbiol 2013;51(11):3835-38.
Lead and corresponding authors
- Kevin Fonseca, Clinical Virologist, Provincial Laboratory, Alberta Health Services, Canada
- Martin Lavoie, Deputy Medical Officer of Health, Alberta Health, Canada
Additional authors in alphabetical order by organization and last name:
- Alberta Health:
- James Talbot, Chief Medical Officer of Health, Alberta Health, Canada
- Alberta Health Services:
- Jeff Fuller, Clinical Microbiologist, Provincial Laboratory, Alberta Health Services, Canada
- Robyn Harrison, Communicable Disease Consultant Workplace Health & Safety, Alberta Health Services
- Mark Joffe, Senior Medical Director, Infection Prevention and Control, Alberta Health Services
- Kanti Pabbaraju, Senior Scientist, Provincial Laboratory, Alberta Health Services, Canada
- Raymond Tellier, Medical Microbiologist, Provincial Laboratory, Alberta Health Services, Canada
- Graham Tipples, Medical Director, Provincial Laboratory, Alberta Health Services, Canada
- Stephen Tsekrekos, Medical Director, Workplace Health & Safety, Alberta Health Services
- Sallene Wong, Scientist, Provincial Laboratory, Alberta Health Services, Canada
- National Microbiology Laboratory:
- Natalie Bastien, Research Scientist, Influenza and Respiratory Virus Section, National Microbiology Laboratory, Winnipeg, Canada
- Yan Li, Chief, Influenza and Respiratory Virus Section, National Microbiology Laboratory, Winnipeg, Canada
Acknowledgments
The named authors would like to acknowledge the timely, thorough and expert contributions made by local medical, nursing, public health, infection control, and health care professionals to this work and this publication. At the request of the family, to preserve confidentiality, additional contributing authors have agreed not to be named. We would also like to express particular thanks to the family for their kind cooperation in this difficult time for them.
--
Kevin Fonseca, PhD, D(ABMM) / Clinical Virologist, Provincial Laboratory of Public Health / Alberta Health Services / Canada kevin.fonseca@albertahealthservices.ca
[ProMED is grateful to Kevin Fonseca and colleagues for providing this authoritative information. This report provides many additional historical, clinical and laboratory details of the recent fatal case of H5N1 influenza in a Canadian traveler returned from Beijing. (Media reports have stated that the patient was a female healthcare worker originally from China, in her 20s.) Notable features include the absence of apparent contact with poultry (though investigation is ongoing), the presence of pneumonia progressing from the right apex to multiple lobes and pleural effusion, the presence of intracranial edema, and radiographic evidence of inflammation of the meninges. It does not appear that influenza was suspected early enough to institute timely antiviral therapy.
H5N1 influenza A virus was detected from respiratory samples and from cerebrospinal fluid by nucleic acid amplification methods. Sequence analysis confirmed the identity of the virus and is indicative of viral features including high-pathogenicity, absence of oseltamivir resistance mutations at position 275, and wild-type affinity for the avian sialic acid receptor. - Mod.LM
A HealthMap/ProMED-mail map can be accessed at: http://healthmap.org/r/1zaU.]
(?)
-
-------




Comment