2009 pandemic influenza A(H1N1) virus in Scotland: geographically variable immunity in Spring 2010, following the winter outbreak (Euro Surveill., abstract, edited)
[Source: EuroSurveillance.org, (LINK). Abstract, full document, edited.]
Eurosurveillance, Volume 15, Issue 24, 17 June 2010
Rapid communications
2009 pandemic influenza A(H1N1) virus in Scotland: geographically variable immunity in Spring 2010, following the winter outbreak
W E Adamson ( )<sup>1</sup>, S Maddi<sup>1</sup>, C Robertson<sup>2</sup><sup>,3</sup>, S McDonagh<sup>4</sup>, P J Molyneaux<sup>5</sup>, K E Templeton<sup>6</sup>, W F Carman<sup>1</sup>
)<sup>1</sup>, S Maddi<sup>1</sup>, C Robertson<sup>2</sup><sup>,3</sup>, S McDonagh<sup>4</sup>, P J Molyneaux<sup>5</sup>, K E Templeton<sup>6</sup>, W F Carman<sup>1</sup>
<hr> Citation style for this article: Adamson WE, Maddi S, Robertson C, McDonagh S, Molyneaux PJ, Templeton KE, Carman WF. 2009 pandemic influenza A(H1N1) virus in Scotland: geographically variable immunity in Spring 2010, following the winter outbreak. Euro Surveill. 2010;15(24):pii=19590. Available online: http://www.eurosurveillance.org/View...rticleId=19590
Date of submission: 03 June 2010
<hr>
We determined the age- and location-specific seroprevalence of antibodies against 2009 pandemic influenza A(H1N1) virus in Scotland following the first two waves of infection. Serum samples collected following the winter outbreak were analysed by microneutralisation assay. The proportion of positive sera varied significantly between cities and, in the case of Inverness, between age groups (with younger adults more likely to be positive than older individuals). This study demonstrates that older people are no longer more likely to have antibodies against the virus than younger adults.
<hr>
The pandemic influenza A(H1N1) virus has been spreading throughout the world since May 2009. The objective of this study was to determine the age- and location-specific seroprevalence of antibodies against 2009 pandemic influenza A(H1N1) virus in Scotland following the first two waves of the pandemic. Although population demographics and contact patterns will vary between countries, this information will assist European public health policy makers in planning for the 2010-11 influenza season.
Methods
Anonymised sera from leftover diagnostic samples taken in March 2010 (subsequently referred to as hospital/general practice (GP) samples) were obtained from biochemistry laboratories in four cities in Scotland: Aberdeen, Edinburgh, Glasgow and Inverness. These biochemistry laboratories receive material from a range of hospital departments as well as from general practices. For each site, samples were categorised by age of patient (20-29, 30-39, 40-49 and over 50 years) and 100 samples of each age group at each site were sent to the West of Scotland Specialist Virology Centre for analysis. The sample size was chosen to have a power of at least 80% to detect a difference of 10% points in seroprevalence between two age groups or between two sites, based upon 400 observations in each site and in each age group. In addition, 100 anonymised sera from leftover diagnostic samples taken in May 2010 in genito-urinary medicine (GUM) clinics in each of the four cities were collected (minimal influenza activity occurred in Scotland between March 2010 and May 2010 [1]), along with a further 128 routine hospital/GP samples from patients in Glasgow aged over 50. Antibody responses were detected by microneutralisation assays, according to standard methods [2]. The virus strain used was the NYMC X-179A reassortant derived from A/California/7/2009 (supplied by the National Institute for Biological Standards and Control, Potters Bar). Each serum sample was tested at a dilution of 1:40, since positivity at this dilution has previously been taken to indicate a significant antibody response [3]. Logistic regression analysis was used to estimate the effect of age group, location, and sample type on prevalence and 95% confidence intervals (CI) are used throughout. As a fixed sample size was used in each location, summary prevalences are based upon a weighted combination of the age and location specific prevalences for a stratified sample. The weights are derived from the population of Scotland in the age groups and catchment areas for the laboratories [4].
Results
Table 1 shows the percentage of hospital/GP samples that were found to be positive for antibodies against 2009 pandemic influenza A(H1N1) virus by age and location. Among these samples there is strong evidence from logistic regression modelling that the age seroprevalence profile is not the same at each site (p=0.0005).
Table 1. Hospital/general practice samples positive for antibodies against
2009 pandemic influenza A(H1N1) virus by age and location, Scotland, March 2010 (n=100 samples per age group in each location)
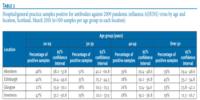
In Aberdeen, Edinburgh and Glasgow there do not appear to be significant intra-site variations in percentage positivity with age. However, in comparison with Aberdeen and Edinburgh, there appears to be lower overall positivity in Glasgow, particularly among younger age groups. To confirm the results for Glasgow, we tested a further 128 hospital/GP samples from patients aged over 50 years and found 41 to be positive (32.0%; 95% CI: 23.9-40.1), compared with 33.0% (95% CI: 23.8?42.2) from the first batch of samples.
The samples obtained from general practices and hospital departments cannot be considered a random sample from the general population as they are likely to have an overrepresentation among patients in groups more likely to receive an influenza vaccination. It is not likely that patients attending GUM clinics are over represented in such groups. The observation of similar levels of seroprevalence among 20-29 year-olds from GUM and hospital/GP samples at each of the four sites (p=0.19) is reassuring for the use of hospital/GP samples to estimate seroprevalence (Table 2).
Table 2. Hospital/general practice and genito-urinary medicine clinical samples from patients aged 20-29 positive for antibodies against 2009 pandemic influenza A(H1N1) virus, Scotland, March 2010

Greater variation in percentage positivity was observed for Inverness, with a decrease in the percentage of positive samples with increased patient age. The geographical area served by the biochemistry laboratory in Inverness is larger, more rural, and considerably less densely populated than the catchment areas for the other biochemistry laboratories utilised in this study. A factor in the higher seroprevalence among 20-29 year-olds compared to those over 50 years old from this area might be mobility: compared with older patients from the same site, 20-29 year-old patients from the Inverness area might be more likely to have travelled, acquired infection from other parts of Scotland, and mixed more with other individuals in their age group.
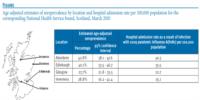
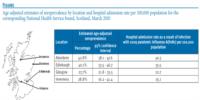
The Figure shows age-adjusted estimates of seroprevalence by location. When the age-adjustment is taken into account, there are higher overall levels of seroprevalence in Aberdeen and Edinburgh than in Glasgow and Inverness. These results appear to correlate with the rates of hospital admission as a result of infection with the virus (calculated from data contained within Health Protection Scotland?s Weekly Influenza Situation Reports [1]). Hospital admission rates as a result of infection with 2009 pandemic influenza A(H1N1) per 100,000 in Grampian (40.3) (the National Health Service board containing Aberdeen) and Lothian (35.5) (Edinburgh) were higher than those in Greater Glasgow and Clyde (22.7) (Glasgow) and Highland (25.1) (Inverness) (Figure). Health Protection Scotland have published influenza-like illness (ILI) and acute respiratory illness (ARI) consultation rates by National Health Service board [1], but these do not show major evidence of regional variation. From the Health Protection Scotland Sentinel Surveillance Scheme (unpublished) there is some evidence that the 2009 pandemic influenza A(H1N1) swab positivity rates in the East of Scotland (which includes Edinburgh) and the North of Scotland (Aberdeen and Inverness) are higher than in the West of Scotland (Glasgow).
Figure. Age-adjusted estimates of seroprevalence by location and hospital admission rate per 100,000 population for the corresponding National Health Service board, Scotland, March 2010
Discussion
Since the outbreak of 2009 pandemic influenza A(H1N1) virus there have been several examinations of the frequency of antibodies against the virus [5 and references therein]. Taken together, these studies are contributing to our understanding of the spread of the virus and providing information that may help in planning future vaccination strategies. While hospital/GP samples cannot be considered to be a random sample from the general population, such samples have previously been used to estimate seroprevalence [3].
A goal of the work described here was to inform public health policy makers in planning for the 2010-11 influenza season. It was felt that this would be done most effectively by making our results available as quickly as possible and as a result the only serum dilution that we have tested to date is 1:40. Microneutralisation assays at this dilution are in line with several other recent analyses of 2009 pandemic influenza A(H1N1) seroprevalence [5].
Recent studies in England, Finland, and Italy examined pre-pandemic serum samples and found that the proportions of samples which contained significant levels of antibodies that are protective against 2009 pandemic influenza A(H1N1) virus increased with age [3,6,7]. During 2009, the burden of the virus was greatest among people aged under 30 years [8]. It has been suggested that older adults were affected less because they were more likely to have previously been exposed to strains with similarities to the new virus.
In Scotland, following the two waves of infection that have occurred so far, it appears that older people are no longer more likely to have significant levels of antibodies than young people. The seroprevalence among young people is, presumably, primarily due to exposure during the two waves of infection. While we currently do not have seroprevalence data for individuals aged under 20 years, the results presented here would suggest that during the 2010-11 influenza season, the burden of infection among adults in Scotland might be similar across age groups, with levels of infection among young adults more in line with those seen in older age groups during 2009.
A weakness of this study is that we do not have any information on the risk group and vaccination status of the patients as only aggregate data, which did not link to any patient characteristics, could be used. This means we are unable to separate out the effect of vaccination from infection or to adjust seroprevalence among the hospital samples for possible selection bias associated with risk groups.
The results presented here will have implications for public health policy in Scotland. Planning for the 2010-11 influenza season should include strategies to target risk groups as a significant proportion of the population remain susceptible to the virus. Glasgow and Inverness have lower overall levels of seroprevalence following the two waves of infection to date, and these cities might experience higher levels of influenza activity than Aberdeen or Edinburgh during the 2010-11 influenza season. The case fatality rate for 2009 pandemic influenza A(H1N1) among individuals aged over 65 years is greater than that observed for seasonal influenza [9]. If the majority of people aged over 50 years remain susceptible, targeting older individuals for vaccination should be a priority. This might be particularly desirable for the Inverness area, where our results indicate particularly high levels of susceptibility among older people.
Acknowledgements
We thank Diane Major, National Institute for Biological Standards and Control, Potters Bar for supplying the influenza virus and control serum used in microneutralisation assays; Ian Collacott, Department of Medical Microbiology, Aberdeen; Matt Noel, Specialist Virology Centre, Edinburgh; Richard Spooner and Ian Pattie, Biochemistry, Gartnavel General Hospital; Anne Pollock, Head of Biochemistry, Raigmore Hospital.
<hr>
References
-
------
[Source: EuroSurveillance.org, (LINK). Abstract, full document, edited.]
Eurosurveillance, Volume 15, Issue 24, 17 June 2010
Rapid communications
2009 pandemic influenza A(H1N1) virus in Scotland: geographically variable immunity in Spring 2010, following the winter outbreak
W E Adamson (
- West of Scotland Specialist Virology Centre, Glasgow, Scotland
- Health Protection Scotland, Glasgow, Scotland
- University of Strathclyde, Glasgow, Scotland
- Microbiology Department, Raigmore Hospital, Inverness, Scotland
- Department of Medical Microbiology, Aberdeen Royal Infirmary, Aberdeen, Scotland
- Edinburgh Specialist Virology Centre, Edinburgh, Scotland
<hr> Citation style for this article: Adamson WE, Maddi S, Robertson C, McDonagh S, Molyneaux PJ, Templeton KE, Carman WF. 2009 pandemic influenza A(H1N1) virus in Scotland: geographically variable immunity in Spring 2010, following the winter outbreak. Euro Surveill. 2010;15(24):pii=19590. Available online: http://www.eurosurveillance.org/View...rticleId=19590
Date of submission: 03 June 2010
<hr>
We determined the age- and location-specific seroprevalence of antibodies against 2009 pandemic influenza A(H1N1) virus in Scotland following the first two waves of infection. Serum samples collected following the winter outbreak were analysed by microneutralisation assay. The proportion of positive sera varied significantly between cities and, in the case of Inverness, between age groups (with younger adults more likely to be positive than older individuals). This study demonstrates that older people are no longer more likely to have antibodies against the virus than younger adults.
<hr>
The pandemic influenza A(H1N1) virus has been spreading throughout the world since May 2009. The objective of this study was to determine the age- and location-specific seroprevalence of antibodies against 2009 pandemic influenza A(H1N1) virus in Scotland following the first two waves of the pandemic. Although population demographics and contact patterns will vary between countries, this information will assist European public health policy makers in planning for the 2010-11 influenza season.
Methods
Anonymised sera from leftover diagnostic samples taken in March 2010 (subsequently referred to as hospital/general practice (GP) samples) were obtained from biochemistry laboratories in four cities in Scotland: Aberdeen, Edinburgh, Glasgow and Inverness. These biochemistry laboratories receive material from a range of hospital departments as well as from general practices. For each site, samples were categorised by age of patient (20-29, 30-39, 40-49 and over 50 years) and 100 samples of each age group at each site were sent to the West of Scotland Specialist Virology Centre for analysis. The sample size was chosen to have a power of at least 80% to detect a difference of 10% points in seroprevalence between two age groups or between two sites, based upon 400 observations in each site and in each age group. In addition, 100 anonymised sera from leftover diagnostic samples taken in May 2010 in genito-urinary medicine (GUM) clinics in each of the four cities were collected (minimal influenza activity occurred in Scotland between March 2010 and May 2010 [1]), along with a further 128 routine hospital/GP samples from patients in Glasgow aged over 50. Antibody responses were detected by microneutralisation assays, according to standard methods [2]. The virus strain used was the NYMC X-179A reassortant derived from A/California/7/2009 (supplied by the National Institute for Biological Standards and Control, Potters Bar). Each serum sample was tested at a dilution of 1:40, since positivity at this dilution has previously been taken to indicate a significant antibody response [3]. Logistic regression analysis was used to estimate the effect of age group, location, and sample type on prevalence and 95% confidence intervals (CI) are used throughout. As a fixed sample size was used in each location, summary prevalences are based upon a weighted combination of the age and location specific prevalences for a stratified sample. The weights are derived from the population of Scotland in the age groups and catchment areas for the laboratories [4].
Results
Table 1 shows the percentage of hospital/GP samples that were found to be positive for antibodies against 2009 pandemic influenza A(H1N1) virus by age and location. Among these samples there is strong evidence from logistic regression modelling that the age seroprevalence profile is not the same at each site (p=0.0005).
Table 1. Hospital/general practice samples positive for antibodies against
2009 pandemic influenza A(H1N1) virus by age and location, Scotland, March 2010 (n=100 samples per age group in each location)
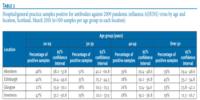
In Aberdeen, Edinburgh and Glasgow there do not appear to be significant intra-site variations in percentage positivity with age. However, in comparison with Aberdeen and Edinburgh, there appears to be lower overall positivity in Glasgow, particularly among younger age groups. To confirm the results for Glasgow, we tested a further 128 hospital/GP samples from patients aged over 50 years and found 41 to be positive (32.0%; 95% CI: 23.9-40.1), compared with 33.0% (95% CI: 23.8?42.2) from the first batch of samples.
The samples obtained from general practices and hospital departments cannot be considered a random sample from the general population as they are likely to have an overrepresentation among patients in groups more likely to receive an influenza vaccination. It is not likely that patients attending GUM clinics are over represented in such groups. The observation of similar levels of seroprevalence among 20-29 year-olds from GUM and hospital/GP samples at each of the four sites (p=0.19) is reassuring for the use of hospital/GP samples to estimate seroprevalence (Table 2).
Table 2. Hospital/general practice and genito-urinary medicine clinical samples from patients aged 20-29 positive for antibodies against 2009 pandemic influenza A(H1N1) virus, Scotland, March 2010

Greater variation in percentage positivity was observed for Inverness, with a decrease in the percentage of positive samples with increased patient age. The geographical area served by the biochemistry laboratory in Inverness is larger, more rural, and considerably less densely populated than the catchment areas for the other biochemistry laboratories utilised in this study. A factor in the higher seroprevalence among 20-29 year-olds compared to those over 50 years old from this area might be mobility: compared with older patients from the same site, 20-29 year-old patients from the Inverness area might be more likely to have travelled, acquired infection from other parts of Scotland, and mixed more with other individuals in their age group.
The Figure shows age-adjusted estimates of seroprevalence by location. When the age-adjustment is taken into account, there are higher overall levels of seroprevalence in Aberdeen and Edinburgh than in Glasgow and Inverness. These results appear to correlate with the rates of hospital admission as a result of infection with the virus (calculated from data contained within Health Protection Scotland?s Weekly Influenza Situation Reports [1]). Hospital admission rates as a result of infection with 2009 pandemic influenza A(H1N1) per 100,000 in Grampian (40.3) (the National Health Service board containing Aberdeen) and Lothian (35.5) (Edinburgh) were higher than those in Greater Glasgow and Clyde (22.7) (Glasgow) and Highland (25.1) (Inverness) (Figure). Health Protection Scotland have published influenza-like illness (ILI) and acute respiratory illness (ARI) consultation rates by National Health Service board [1], but these do not show major evidence of regional variation. From the Health Protection Scotland Sentinel Surveillance Scheme (unpublished) there is some evidence that the 2009 pandemic influenza A(H1N1) swab positivity rates in the East of Scotland (which includes Edinburgh) and the North of Scotland (Aberdeen and Inverness) are higher than in the West of Scotland (Glasgow).
Figure. Age-adjusted estimates of seroprevalence by location and hospital admission rate per 100,000 population for the corresponding National Health Service board, Scotland, March 2010
Discussion
Since the outbreak of 2009 pandemic influenza A(H1N1) virus there have been several examinations of the frequency of antibodies against the virus [5 and references therein]. Taken together, these studies are contributing to our understanding of the spread of the virus and providing information that may help in planning future vaccination strategies. While hospital/GP samples cannot be considered to be a random sample from the general population, such samples have previously been used to estimate seroprevalence [3].
A goal of the work described here was to inform public health policy makers in planning for the 2010-11 influenza season. It was felt that this would be done most effectively by making our results available as quickly as possible and as a result the only serum dilution that we have tested to date is 1:40. Microneutralisation assays at this dilution are in line with several other recent analyses of 2009 pandemic influenza A(H1N1) seroprevalence [5].
Recent studies in England, Finland, and Italy examined pre-pandemic serum samples and found that the proportions of samples which contained significant levels of antibodies that are protective against 2009 pandemic influenza A(H1N1) virus increased with age [3,6,7]. During 2009, the burden of the virus was greatest among people aged under 30 years [8]. It has been suggested that older adults were affected less because they were more likely to have previously been exposed to strains with similarities to the new virus.
In Scotland, following the two waves of infection that have occurred so far, it appears that older people are no longer more likely to have significant levels of antibodies than young people. The seroprevalence among young people is, presumably, primarily due to exposure during the two waves of infection. While we currently do not have seroprevalence data for individuals aged under 20 years, the results presented here would suggest that during the 2010-11 influenza season, the burden of infection among adults in Scotland might be similar across age groups, with levels of infection among young adults more in line with those seen in older age groups during 2009.
A weakness of this study is that we do not have any information on the risk group and vaccination status of the patients as only aggregate data, which did not link to any patient characteristics, could be used. This means we are unable to separate out the effect of vaccination from infection or to adjust seroprevalence among the hospital samples for possible selection bias associated with risk groups.
The results presented here will have implications for public health policy in Scotland. Planning for the 2010-11 influenza season should include strategies to target risk groups as a significant proportion of the population remain susceptible to the virus. Glasgow and Inverness have lower overall levels of seroprevalence following the two waves of infection to date, and these cities might experience higher levels of influenza activity than Aberdeen or Edinburgh during the 2010-11 influenza season. The case fatality rate for 2009 pandemic influenza A(H1N1) among individuals aged over 65 years is greater than that observed for seasonal influenza [9]. If the majority of people aged over 50 years remain susceptible, targeting older individuals for vaccination should be a priority. This might be particularly desirable for the Inverness area, where our results indicate particularly high levels of susceptibility among older people.
Acknowledgements
We thank Diane Major, National Institute for Biological Standards and Control, Potters Bar for supplying the influenza virus and control serum used in microneutralisation assays; Ian Collacott, Department of Medical Microbiology, Aberdeen; Matt Noel, Specialist Virology Centre, Edinburgh; Richard Spooner and Ian Pattie, Biochemistry, Gartnavel General Hospital; Anne Pollock, Head of Biochemistry, Raigmore Hospital.
<hr>
References
- Health Protection Scotland (HPS) [Internet]. Glasgow: HPS. Weekly Influenza Situation report (Including H1N1v Archive). Available from: http://www.hps.scot.nhs.uk/resp/swin...zareports.aspx
- Rowe T, Abernathy RA, Hu-Primmer J, Thompson WW, Lu X, Lim W, et al. Detection of antibody to avian influenza A (H5N1) virus in human serum by using a combination of serologic assays. J. Clin. Microbiol. 1999;37(4):937-43.
- Miller E, Hoschler K, Hardelid P, Stanford E, Andrews N, Zambon M. Incidence of 2009 pandemic influenza A H1N1 infection in England: a cross-sectional serological study. Lancet. 2010;375(9720):1100-8.
- Lehtonen, R, Pahkinen E. Practical Methods for Design and Analysis of Complex Surveys. 2nd Edition. New York: Wiley; 2003.
- World Health Organization (WHO). Weekly epidemiological record. 2010:85(24):229-36. Available from: http://www.who.int/wer/2010/wer8524.pdf
- Ikonen N, Strengell M, Kinnunen L, ?sterlund P, Pirhonen J, Broman M, et al. High frequency of cross-reacting antibodies against 2009 pandemic influenza A(H1N1) virus among the elderly in Finland. Euro Surveill. 2010;15(5):pii=19478. Available from: http://www.eurosurveillance.org/View...rticleId=19478
- Rizzo C, Rota MC, Bella A, Alfonsi V, Declich S, Caporali MG, et al. Cross-reactive antibody responses to the 2009 A/H1N1v influenza virus in the Italian population in the pre-pandemic period. Vaccine. 2010:28(20):3558-62.
- Reichert T, Chowell G, Nishiura H, Christensen RA, McCullers JA. Does glycosylation as a modifier of original antigenic sin explain the case age distribution and unusual toxicity in pandemic novel H1N1 influenza? BMC Infect. Dis. 2010:10(5).
- Donaldson LJ, Rutter PD, Ellis BM, Greaves FEC, Mytton OT, Pebody RG, et al. Mortality from pandemic A/H1N1 2009 influenza in England: public health surveillance study. BMJ. 2009.339:b5213.
-
------