2015-2016 Influenza Season Week 6 ending February 13, 2016
All data are preliminary and may change as more reports are received.
Synopsis:
During week 6 (February 7-13, 2016), influenza activity increased in the United States.
*HHS regions (Region 1 CT, ME, MA, NH, RI, VT; Region 2: NJ, NY, Puerto Rico, US Virgin Islands; Region 3: DE, DC, MD, PA, VA, WV; Region 4: AL, FL, GA, KY, MS, NC, SC, TN; Region 5: IL, IN, MI, MN, OH, WI; Region 6: AR, LA, NM, OK, TX; Region 7: IA, KS, MO, NE; Region 8: CO, MT, ND, SD, UT, WY; Region 9: AZ, CA, Guam, HI, NV; and Region 10: AK, ID, OR, WA).
? Elevated means the % of visits for ILI is at or above the national or region-specific baseline
§ Includes all 50 states, New York City, the District of Columbia and Puerto Rico
? National data are for current week; regional data are for the most recent three weeks
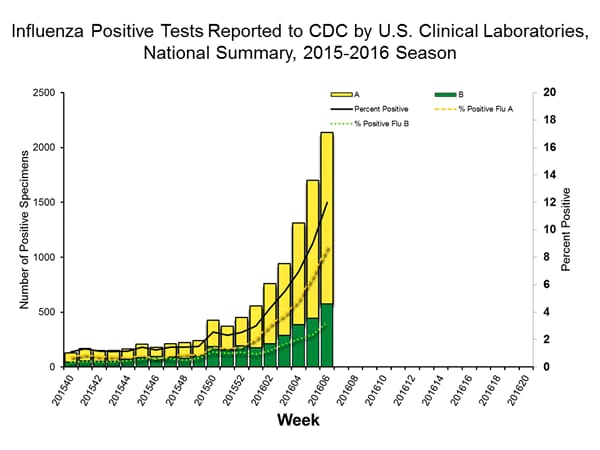
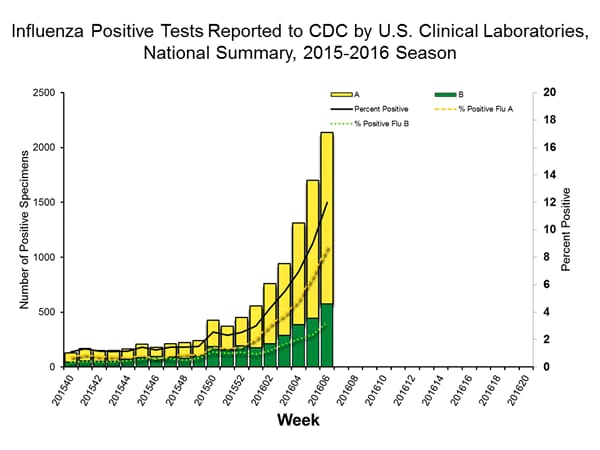
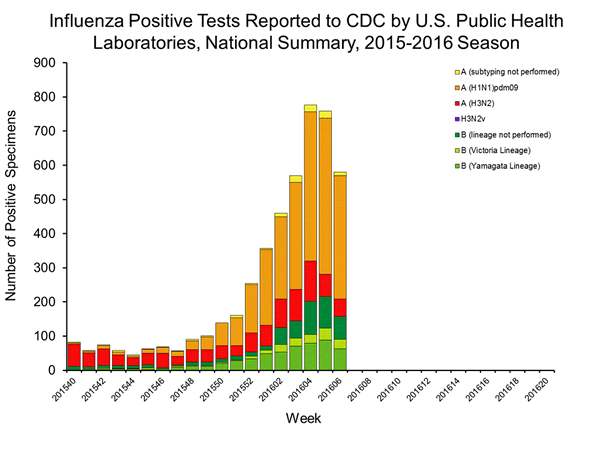
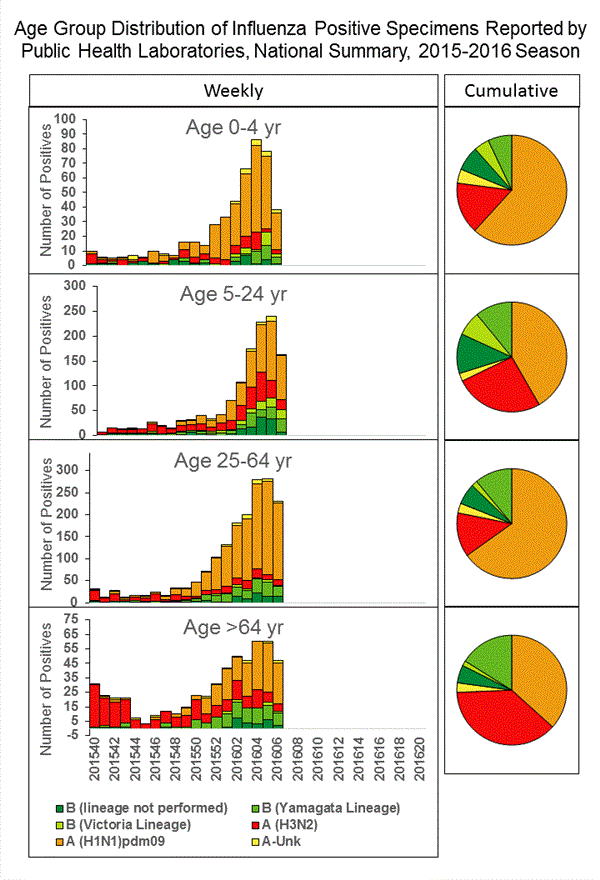
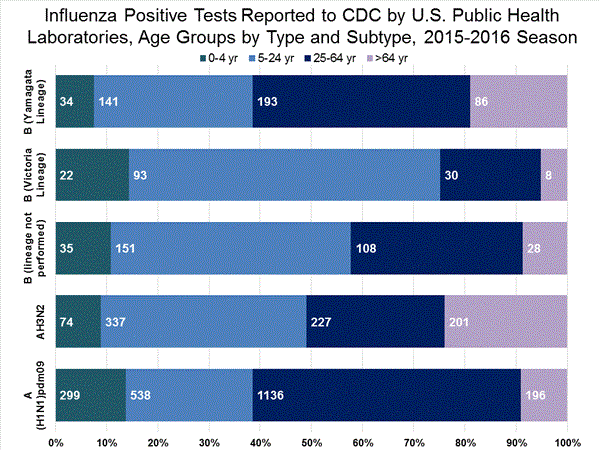
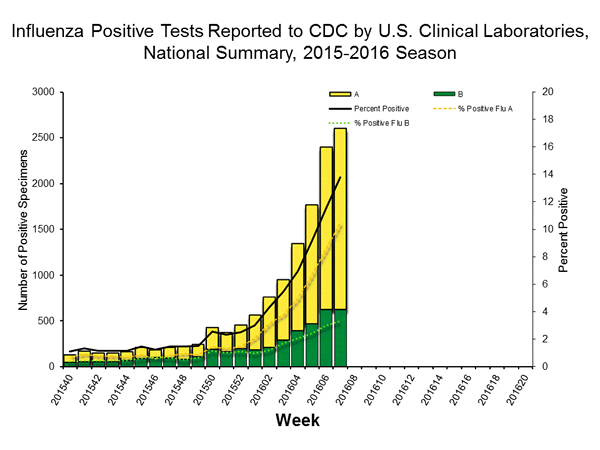
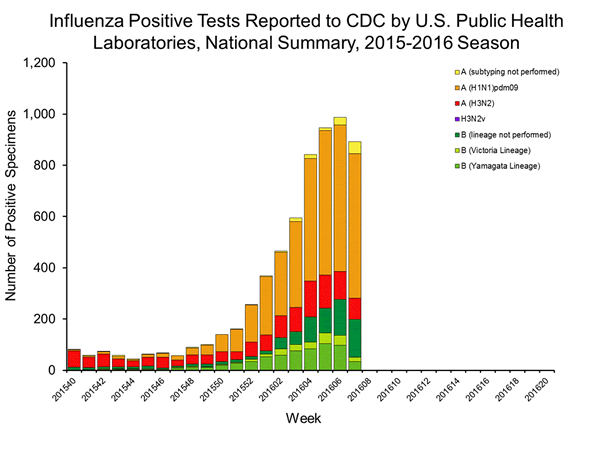
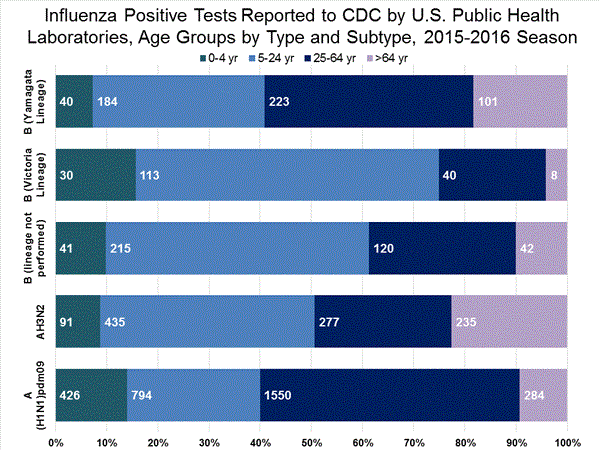
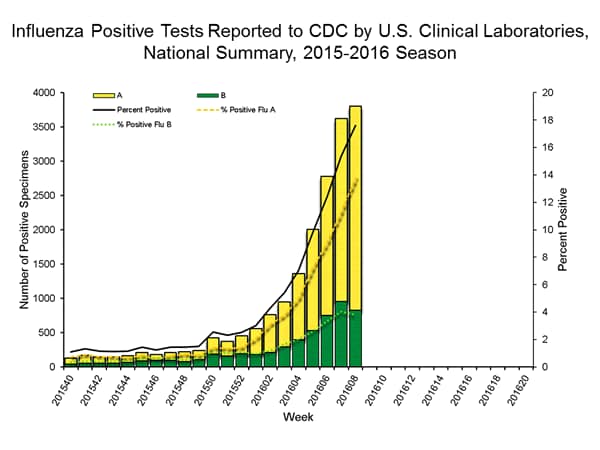
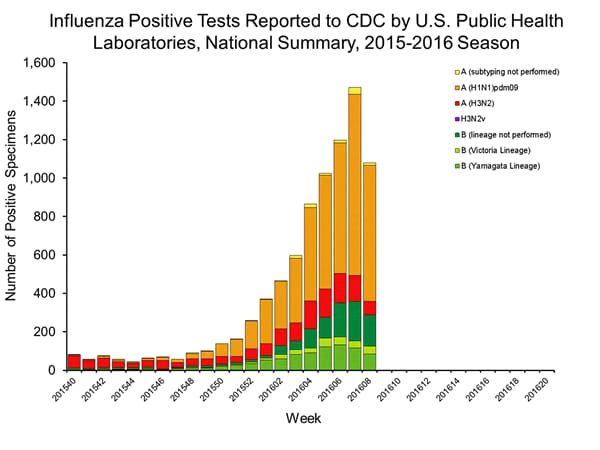
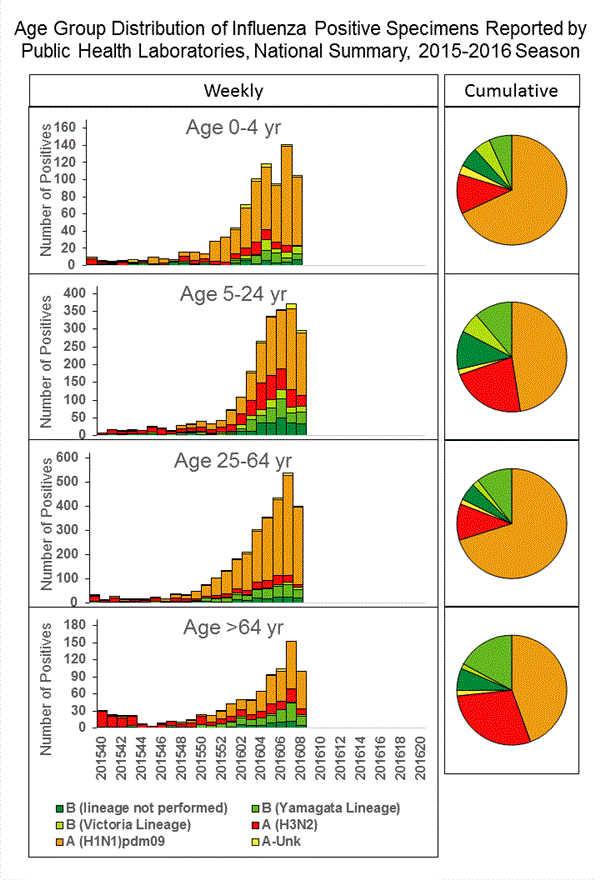
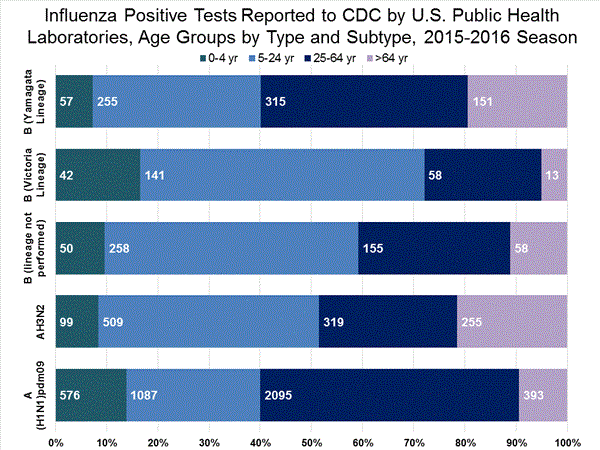
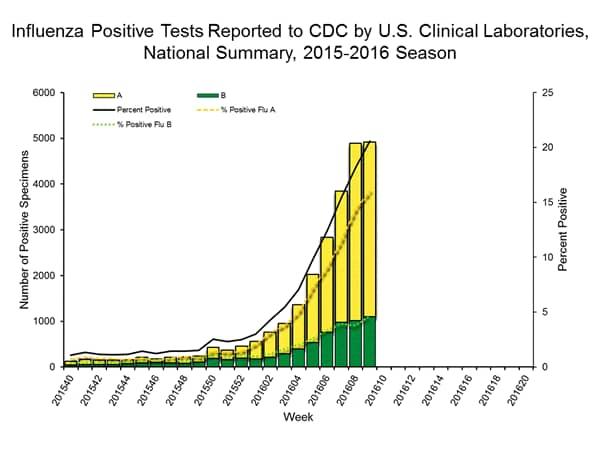
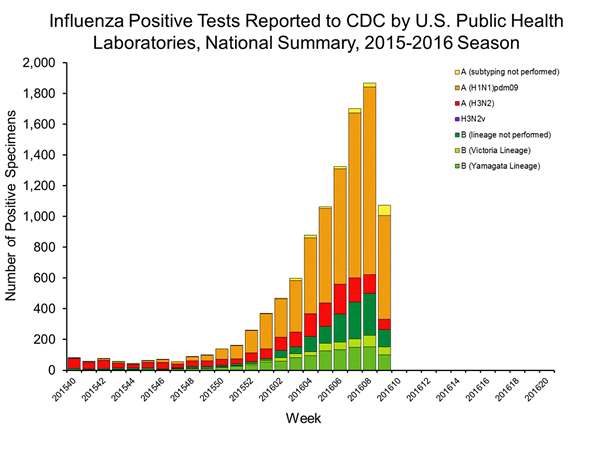
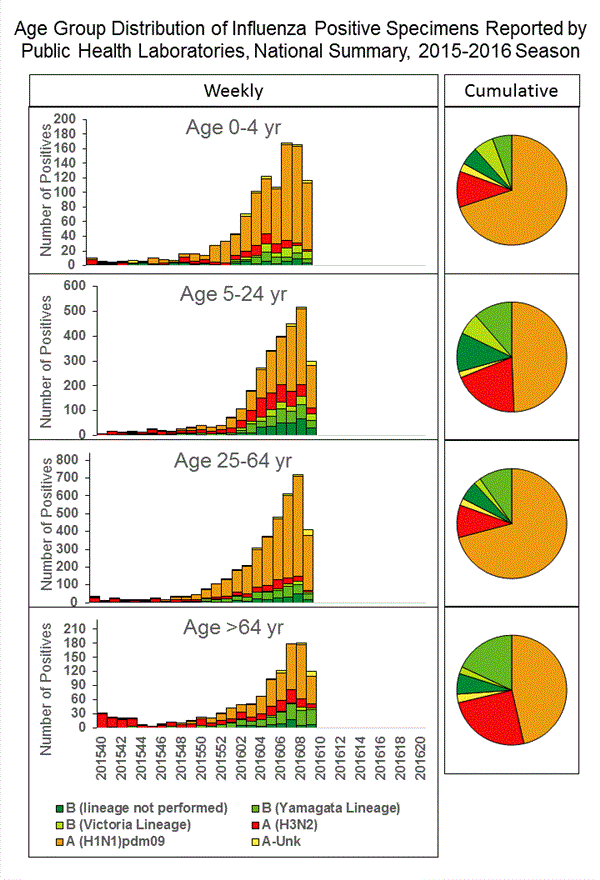
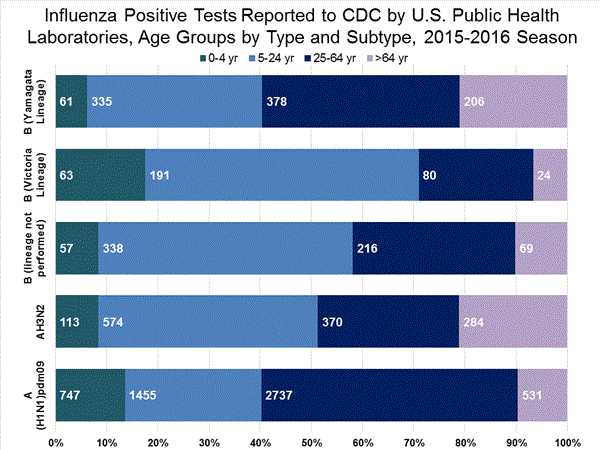
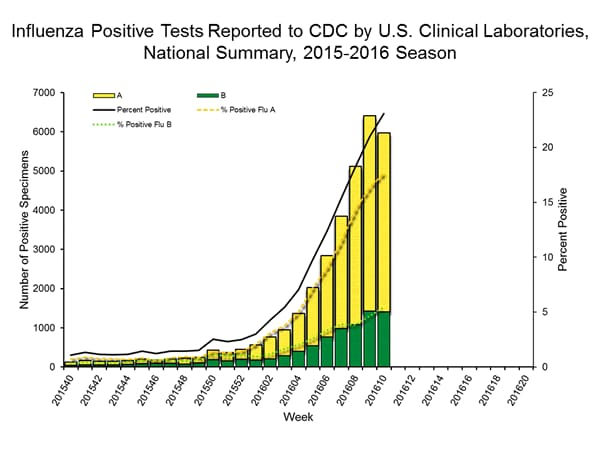
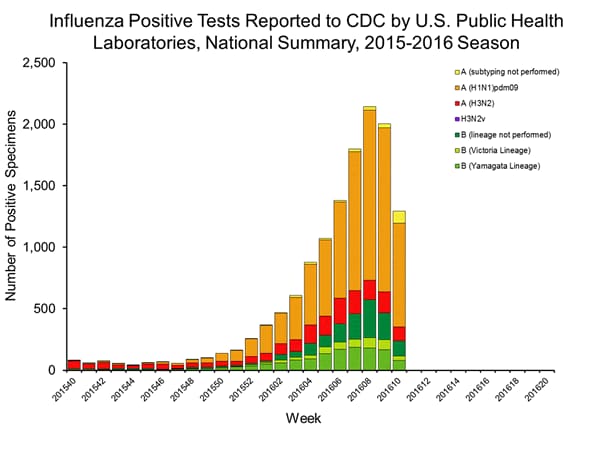
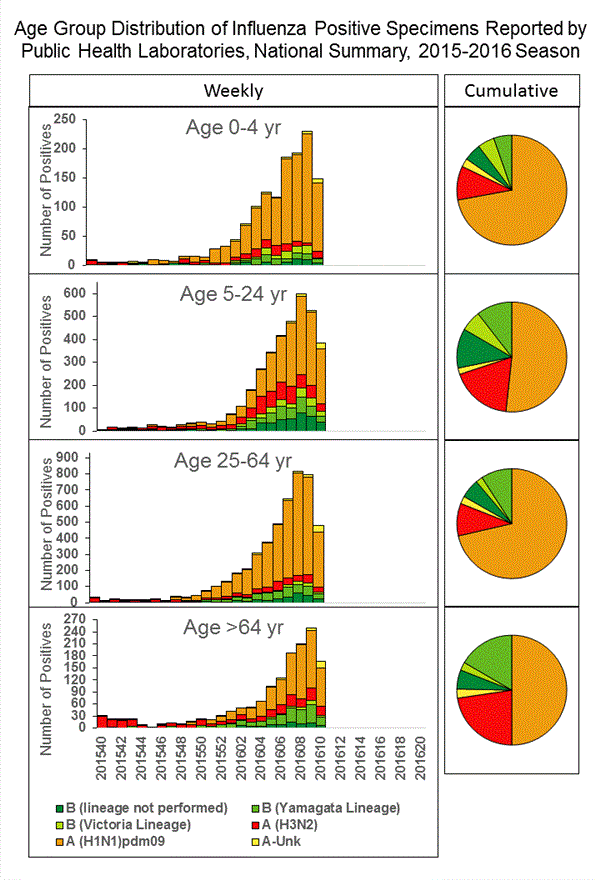
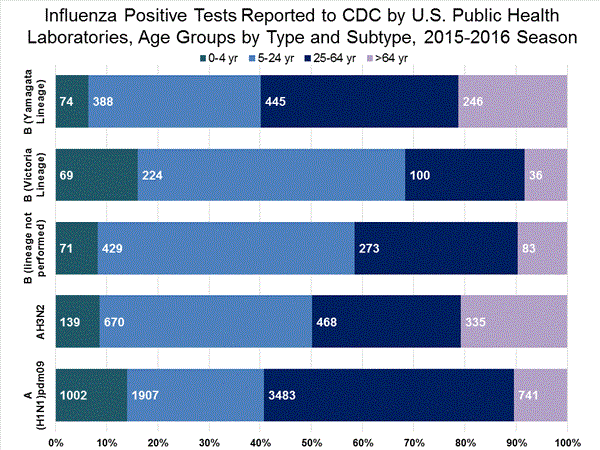
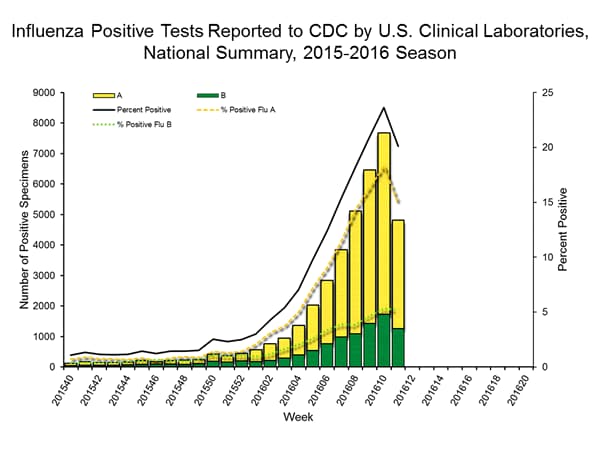
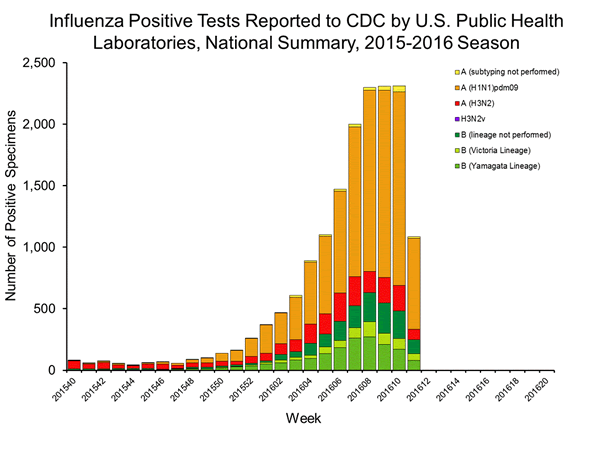
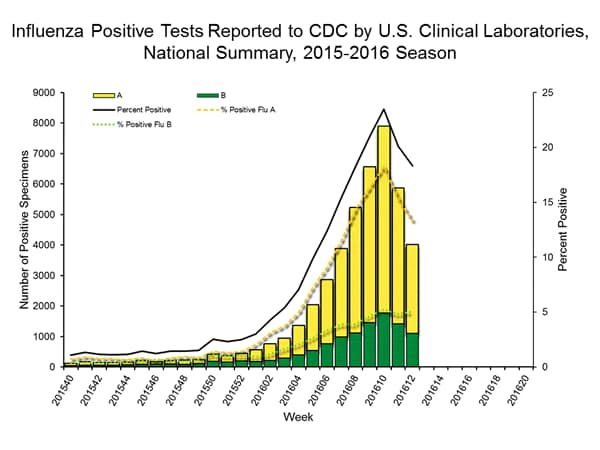
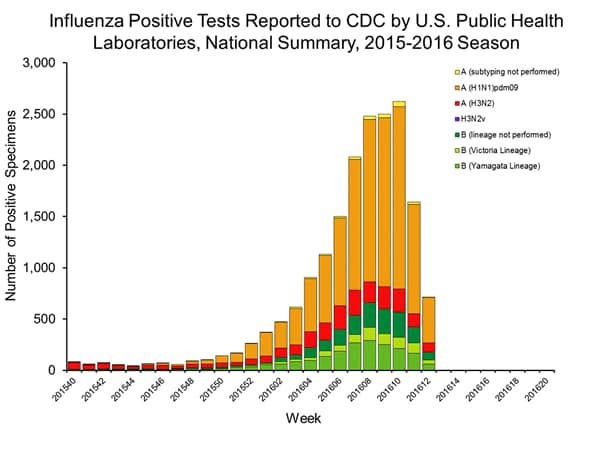
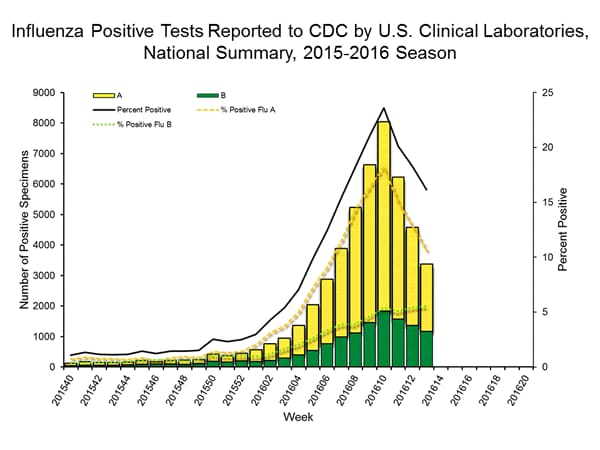
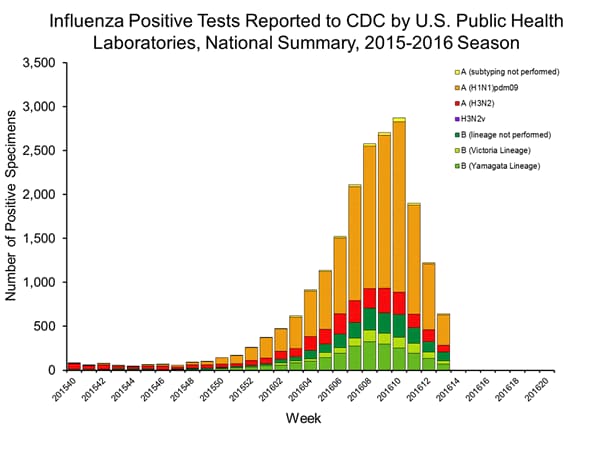
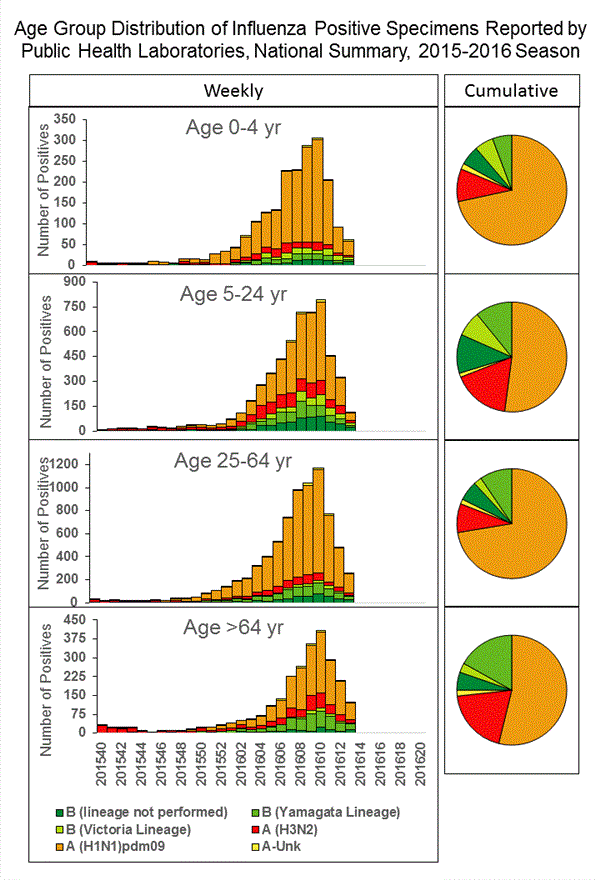
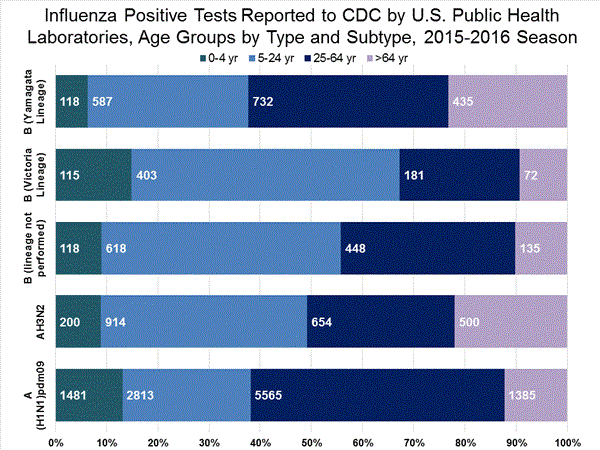
U.S. Virologic Surveillance:
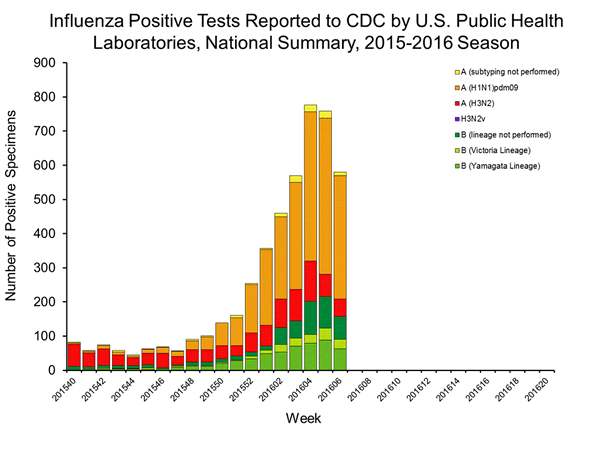
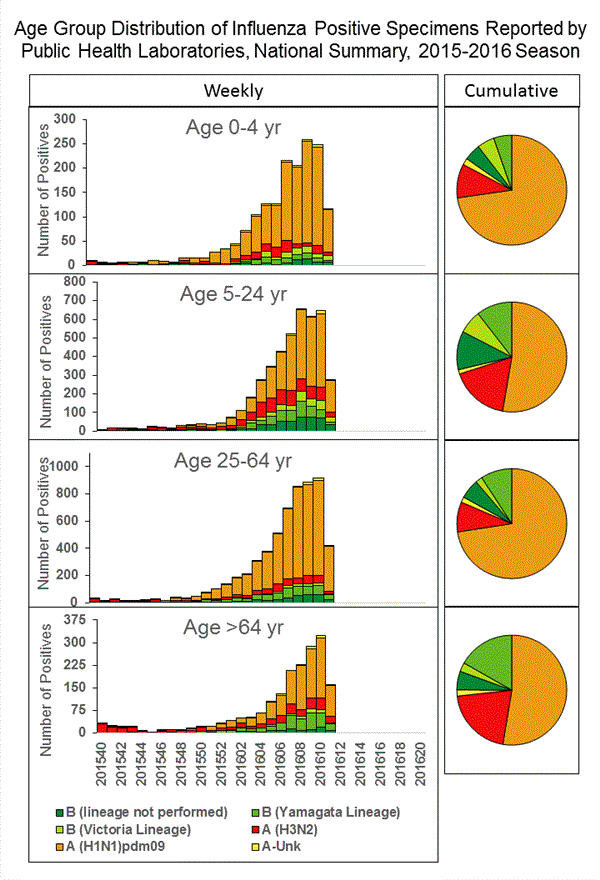
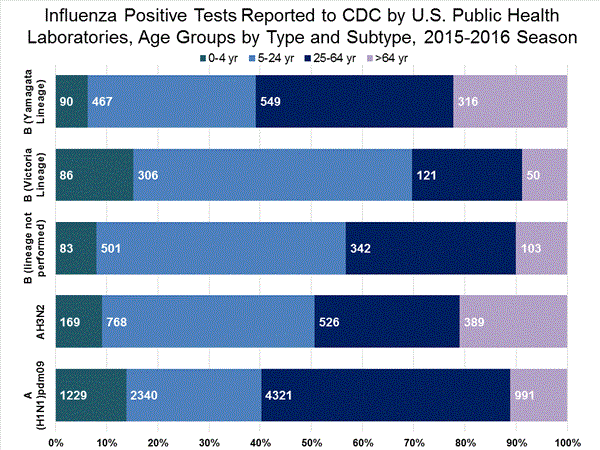
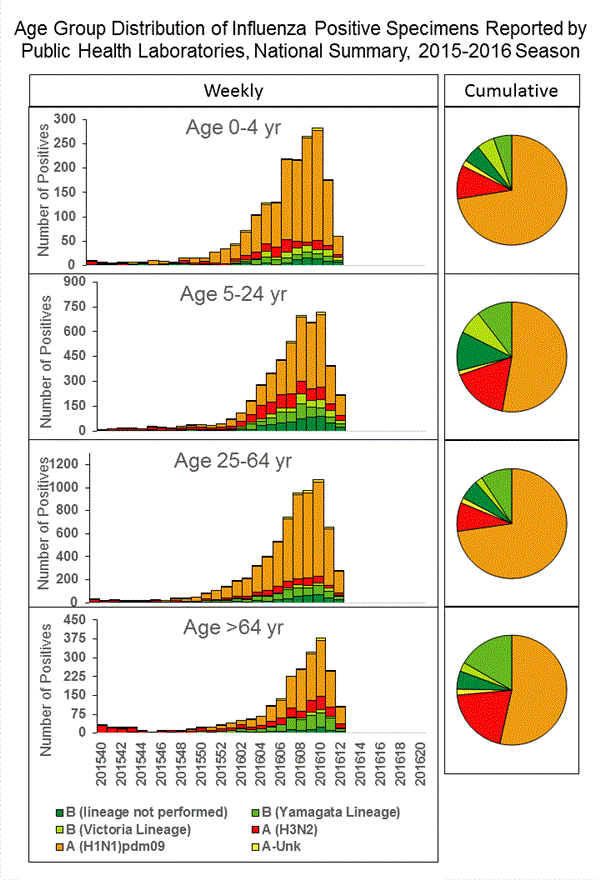
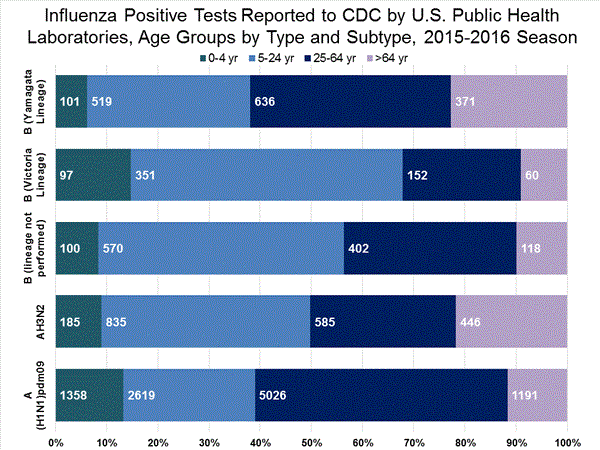
WHO and NREVSS collaborating laboratories, which include both public health and clinical laboratories located in all 50 states, Puerto Rico, and the District of Columbia, report to CDC the total number of respiratory specimens tested for influenza and the number positive for influenza by virus type. In addition, public health laboratories also report the influenza A subtype (H1 or H3) and influenza B lineage information of the viruses they test and the age or age group of the persons from whom the specimens were collected.
Additional data are available at http://gis.cdc.gov/grasp/fluview/flu...dashboard.html.
The results of tests performed by clinical laboratories during the current week are summarized below.
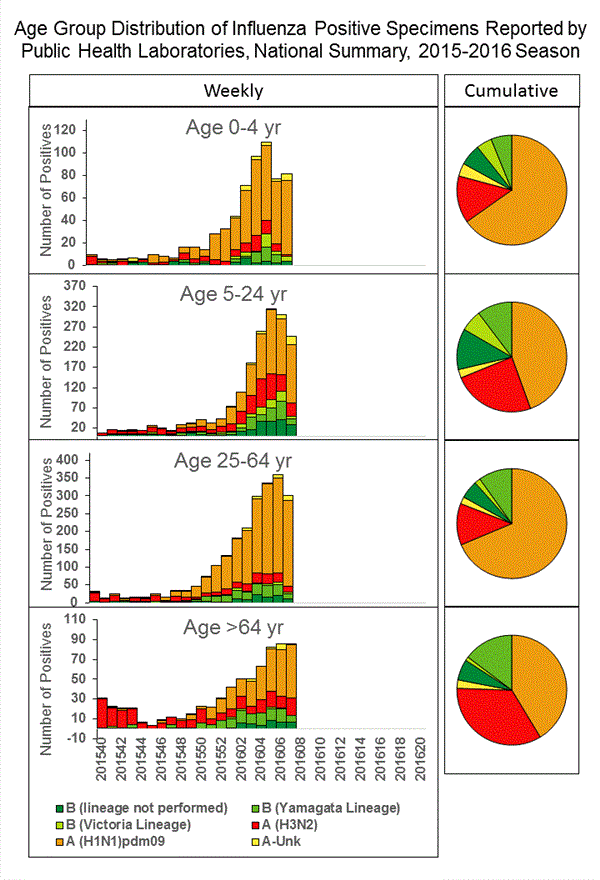
View National and Regional Level Graphs and Data | View Chart Data | View Full Screen | View PowerPoint Presentation The results of tests performed by public health laboratories, as well as the age group distribution of influenza positive tests, during the current week are summarized below.
*The percent of specimens testing positive for influenza is not reported because public health laboratories often receive samples that have already tested positive for influenza at a clinical laboratory and therefore percent positive would not be a valid indicator of influenza activity. Additional information is available at http://www.cdc.gov/flu/weekly/overview.htm.
View National and Regional Level Graphs and Data | View Chart Data | View Full Screen | View PowerPoint Presentation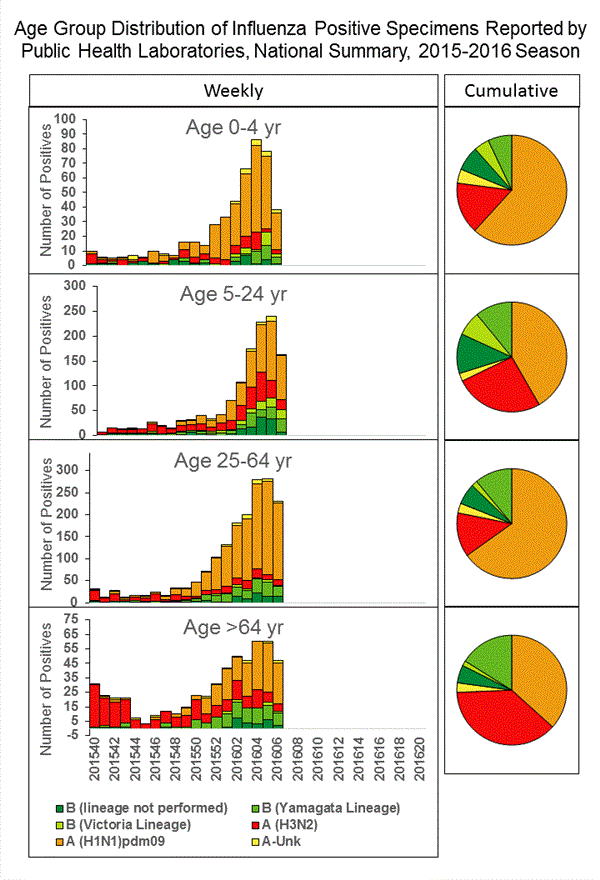
View Chart Data | View Full Screen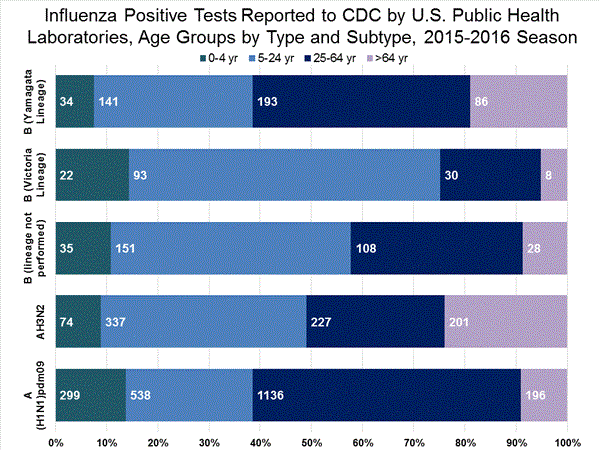
View Chart Data |View Full Screen Influenza Virus Characterization:
CDC characterizes influenza viruses through one or more tests including genome sequencing, hemagglutination inhibition (HI) and/or neutralization assays. These data are used to compare how similar currently circulating influenza viruses are to the reference viruses used for developing influenza vaccines, and to monitor for changes in circulating influenza viruses. Historically, HI data have been used most commonly to assess the similarity between reference viruses and circulating viruses to suggest how well the vaccine may work until such time as vaccine effectiveness estimates are available. During the 2014–2015 season and to date, however, a portion of influenza A (H3N2) viruses do not yield sufficient hemagglutination titers for antigenic characterization by HI. For many of these viruses, CDC performs genetic characterization to determine the genetic group identity of those viruses. In this way, antigenic properties of these viruses can be inferred from viruses within the same genetic group that have been characterized antigenically.
CDC has characterized 532 influenza viruses [181 A (H1N1)pdm09, 228 A (H3N2), and 123 influenza B viruses] collected by U.S. laboratories since October 1, 2015.
Influenza A Virus [409]
Testing of influenza A(H1N1)pdm09, A(H3N2), and influenza B virus isolates for resistance to neuraminidase inhibitors (oseltamivir, zanamivir, and peramivir) is performed at CDC using a functional assay. Additional A(H1N1)pdm09 and A(H3N2) clinical samples are tested for mutations of the virus known to confer oseltamivir resistance. The data summarized below combine the results of both testing methods. These samples are routinely obtained for surveillance purposes rather than for diagnostic testing of patients suspected to be infected with antiviral-resistant virus.
High levels of resistance to the adamantanes (amantadine and rimantadine) persist among A(H1N1)pdm09 and A(H3N2) viruses (the adamantanes are not effective against influenza B viruses). Therefore, data from adamantane resistance testing are not presented below.
The majority of recently circulating influenza viruses are susceptible to the neuraminidase inhibitor antiviral medications, oseltamivir, zanamivir, and peramivir; however, rare sporadic instances of oseltamivir-resistant and peramivir-resistant influenza A (H1N1)pdm09 viruses and oseltamivir-resistant influenza A (H3N2) viruses have been detected worldwide. Antiviral treatment as early as possible is recommended for patients with confirmed or suspected influenza who have severe, complicated, or progressive illness; who require hospitalization; or who are at high risk. for serious influenza-related complications. Additional information on recommendations for treatment and chemoprophylaxis of influenza virus infection with antiviral agents is available athttp://www.cdc.gov/flu/antivirals/index.htm.
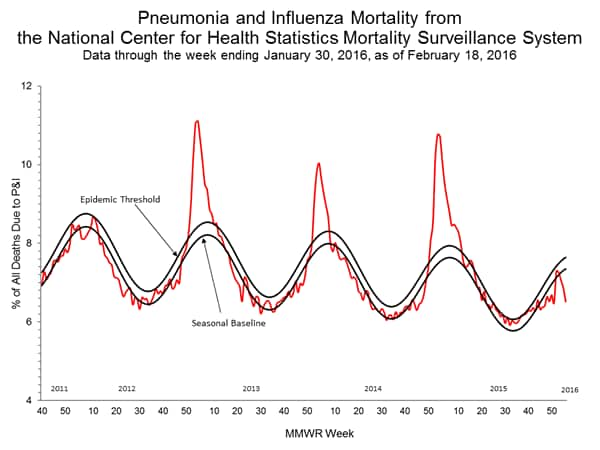
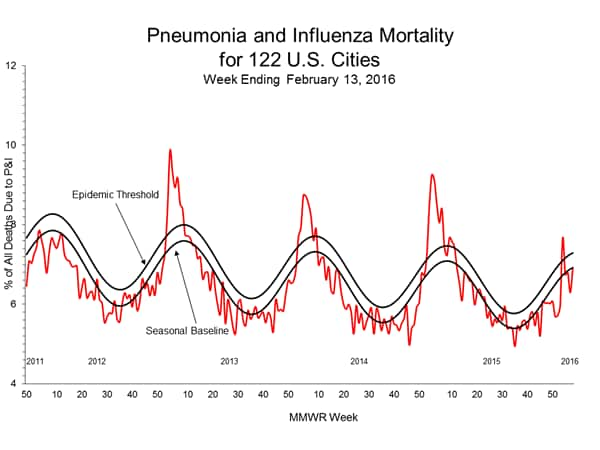
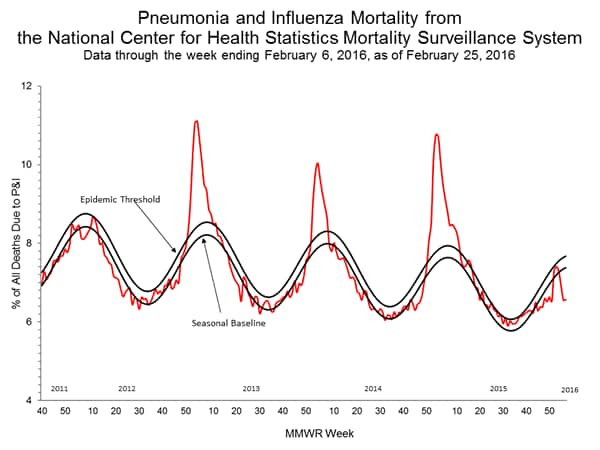
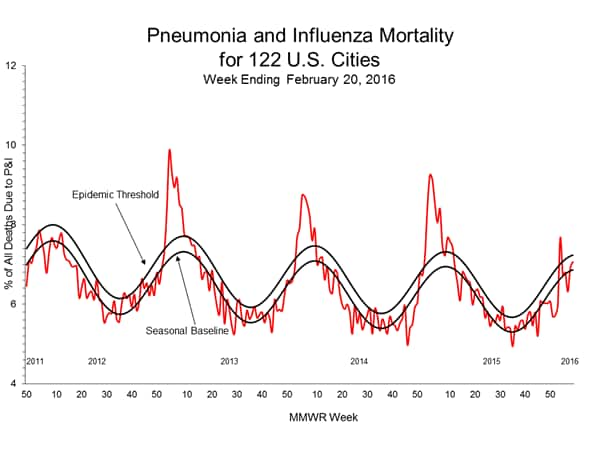
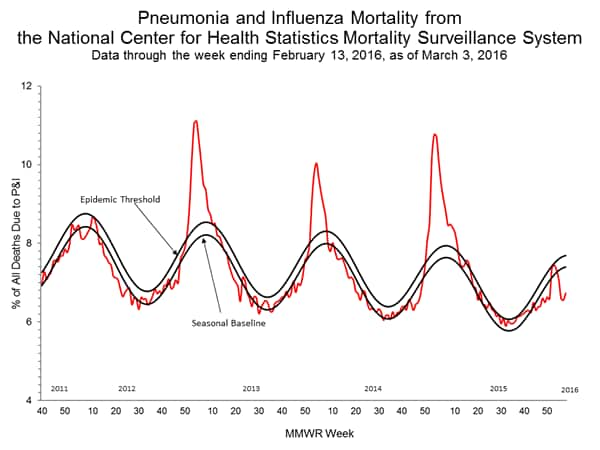
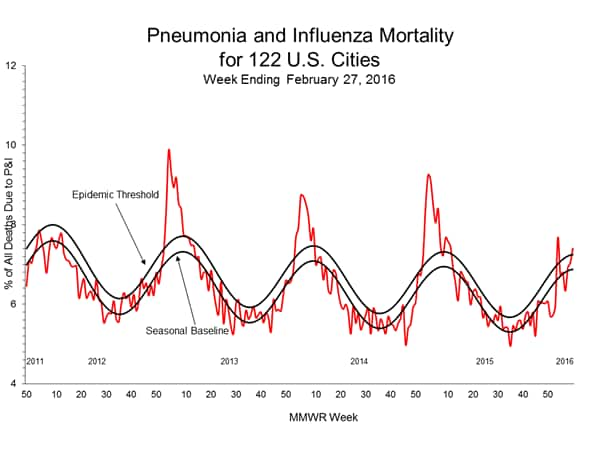
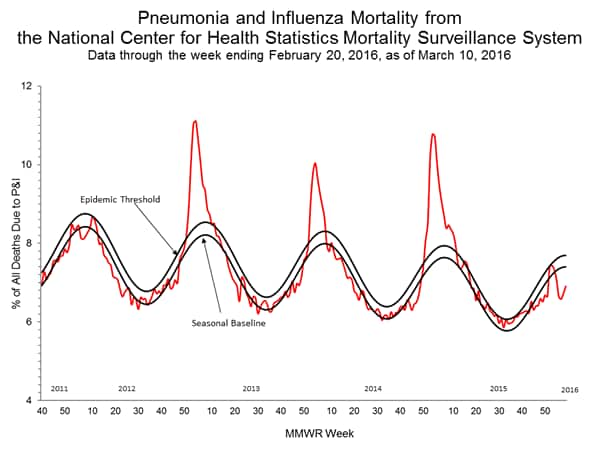
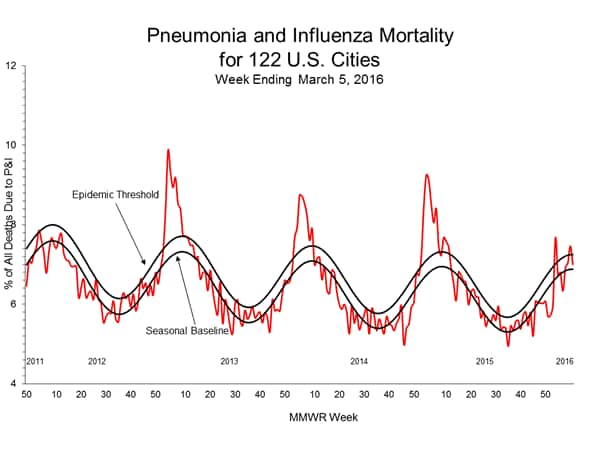
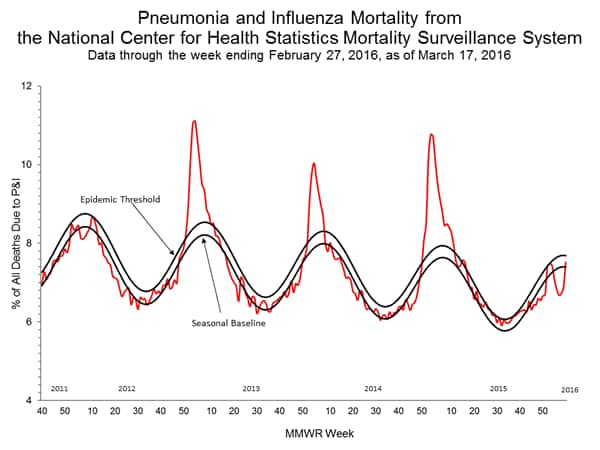
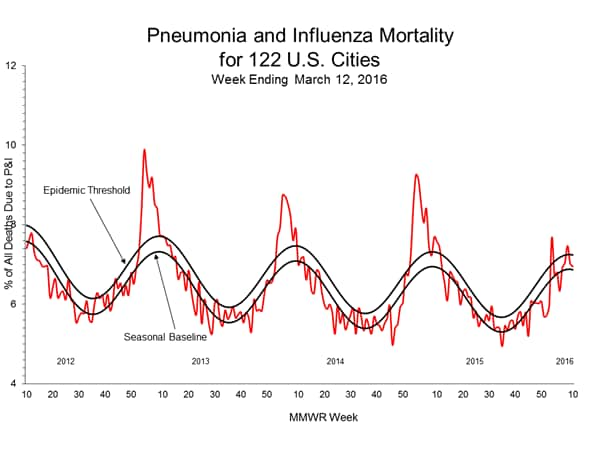
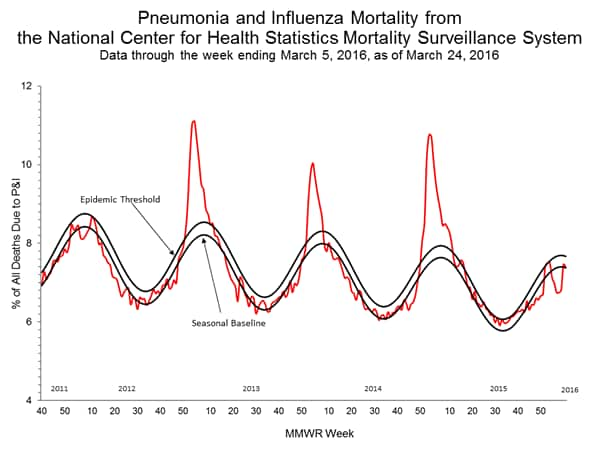
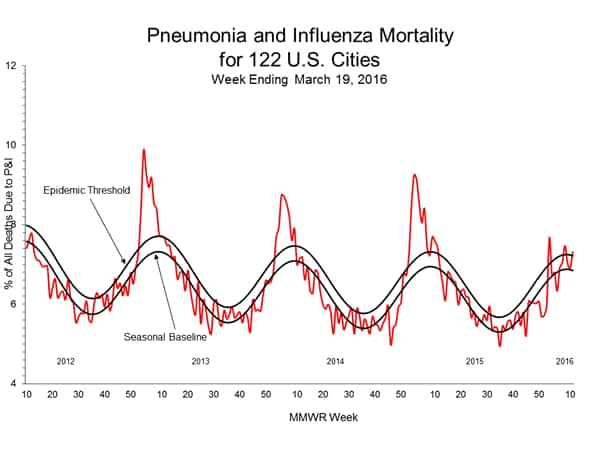
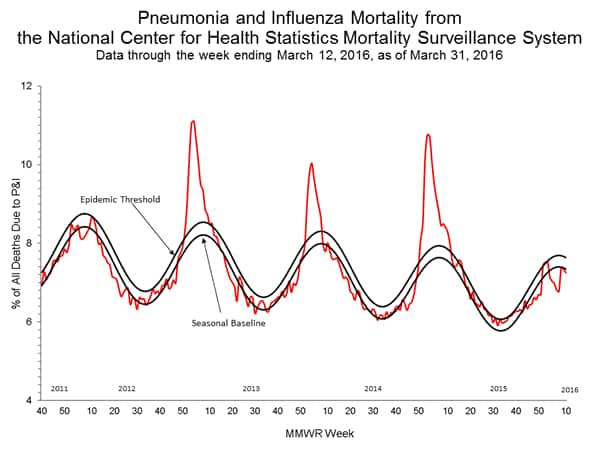
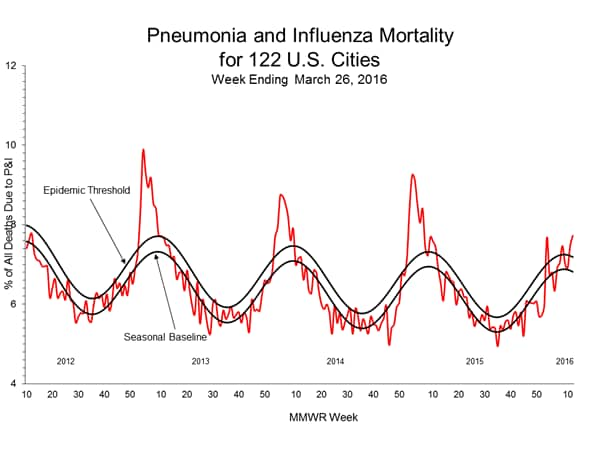
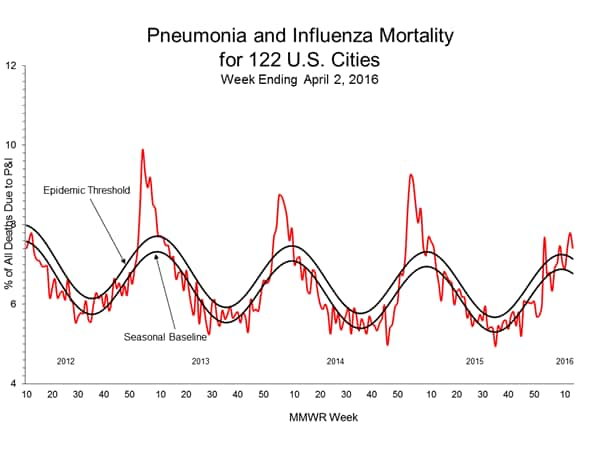
Pneumonia and Influenza (P&I) Mortality Surveillance:
Rapid tracking of pneumonia and influenza-associated deaths is done through two systems, the National Center for Health Statistics (NCHS) Mortality Surveillance System and the 122 Cities Mortality Reporting System. NCHS mortality surveillance data are presented by the week the death occurred and P&I percentages are released two weeks after the week of death to allow for collection of enough data to produce a stable P&I percentage. Users of the data should not expect the two systems to produce the same percentages, and the percent P&I deaths from each system should be compared to the corresponding system-specific baselines and thresholds.
NCHS Mortality Surveillance Data:
Based on NCHS mortality surveillance data available on February 18, 2016, 6.5% of the deaths occurring during the week ending January 30, 2016 (week 4) were due to P&I. This percentage is below the epidemic threshold of 7.6% for week 4.
Region and state-specific data are available at http://www.cdc.gov/flu/weekly/nchs.htm.
View Regional and State Level Data | View Chart Data | View Full Screen | View PowerPoint Presentation 122 Cities Mortality Reporting System:
During week 6, 6.9% of all deaths reported through the 122 Cities Mortality Reporting System were due to P&I. This percentage was below the epidemic threshold of 7.3% for week 6.
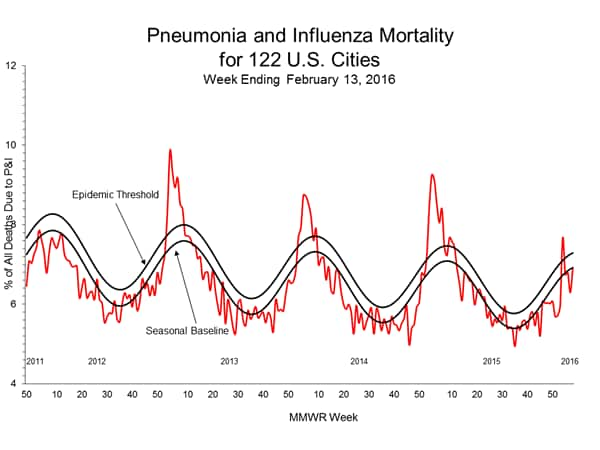
View Full Screen | View PowerPoint Presentation
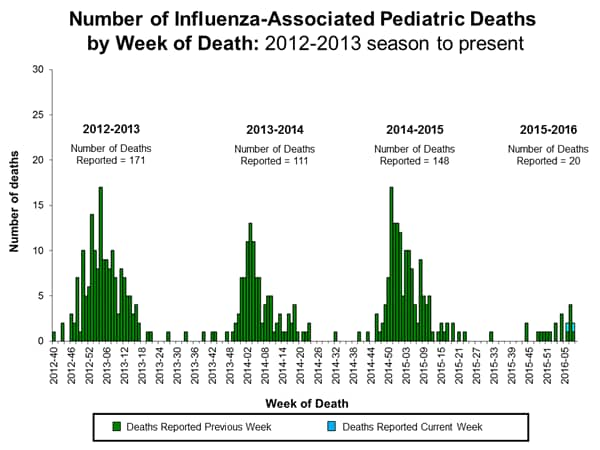
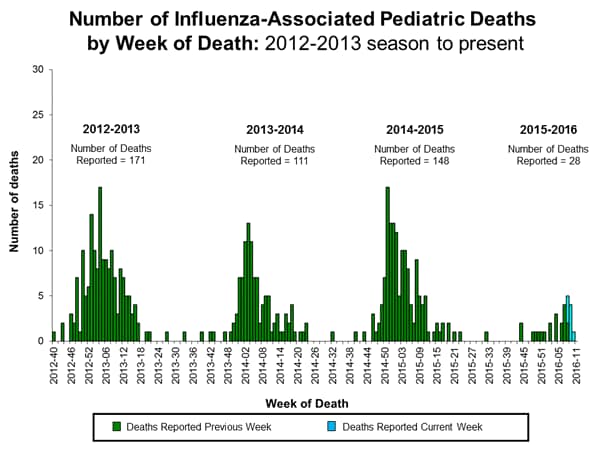
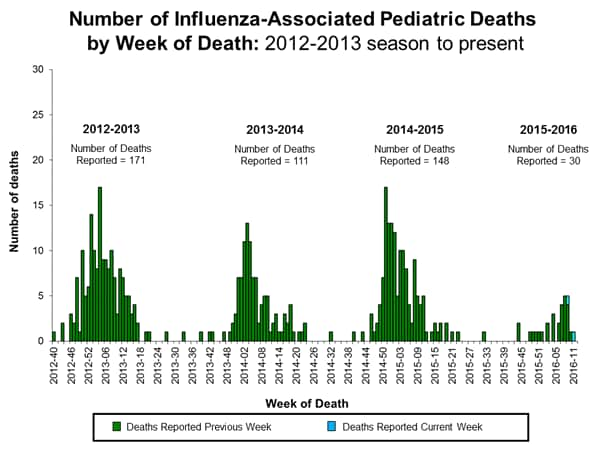
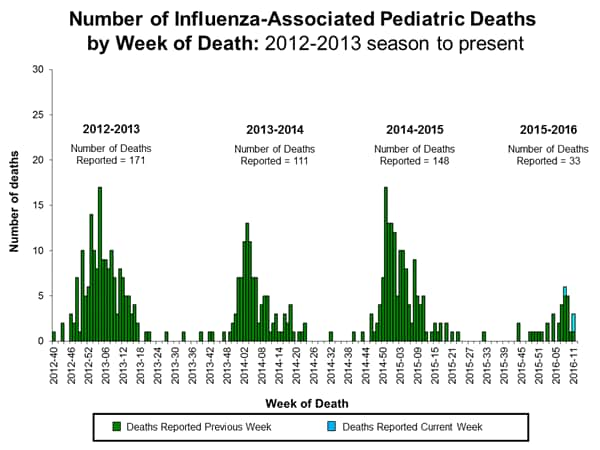
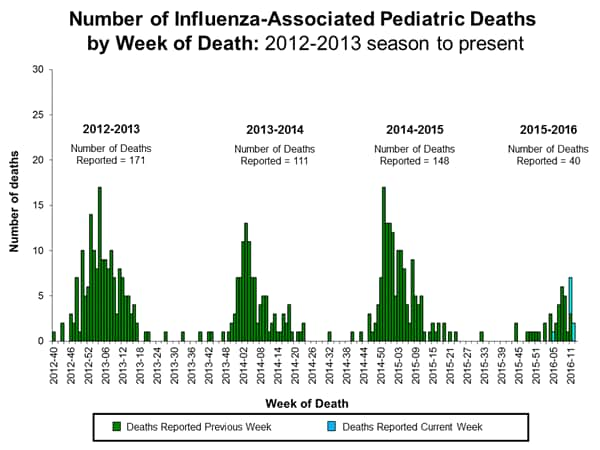
Influenza-Associated Pediatric Mortality:
Two influenza-associated pediatric deaths were reported to CDC during week 6. One death was associated with an influenza A (H1N1)pdm09 virus and occurred during week 2 (the week ending January 16, 2016). One death was associated with an influenza virus for which the type was not determined and occurred during week 6 (the week ending February 13, 2016).
A total of 13 influenza-associated pediatric deaths have been reported during the 2015-2016 season from Puerto Rico [1], Chicago [1], and eight states (Arizona [1], California [2], Florida [3], Louisiana [1], Michigan [1], Nevada [1], Tennessee [1], and Washington [1]).
Additional data can be found at: http://gis.cdc.gov/GRASP/Fluview/PedFluDeath.html.
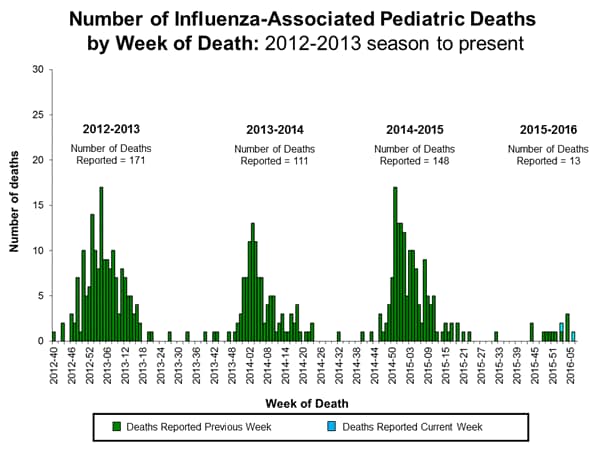
View Interactive Application | View Full Screen | View PowerPoint Presentation
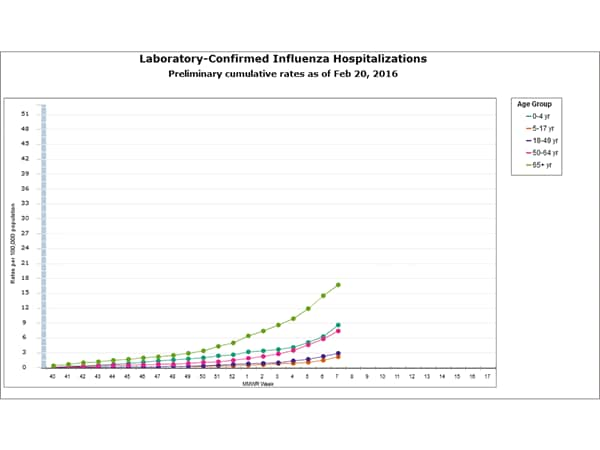
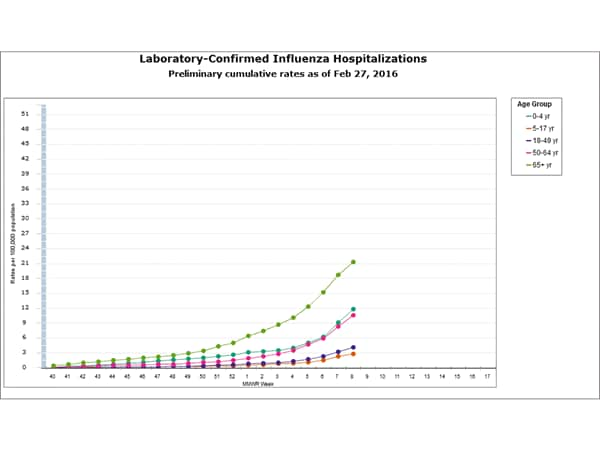
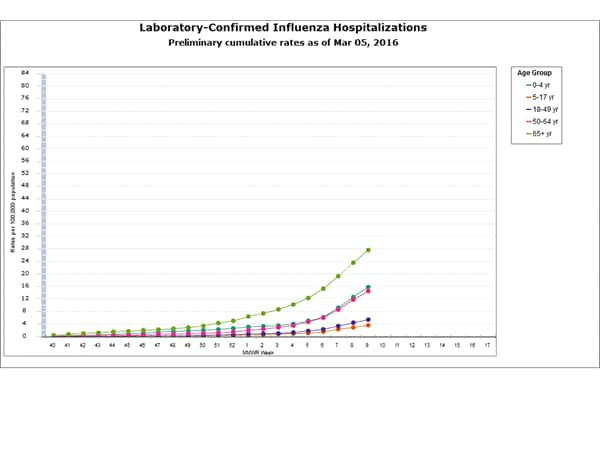
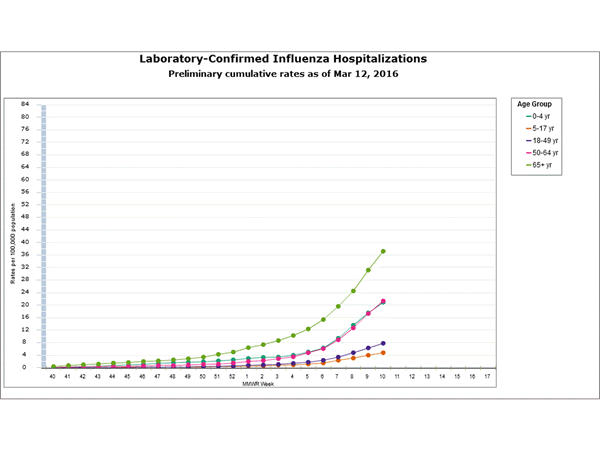
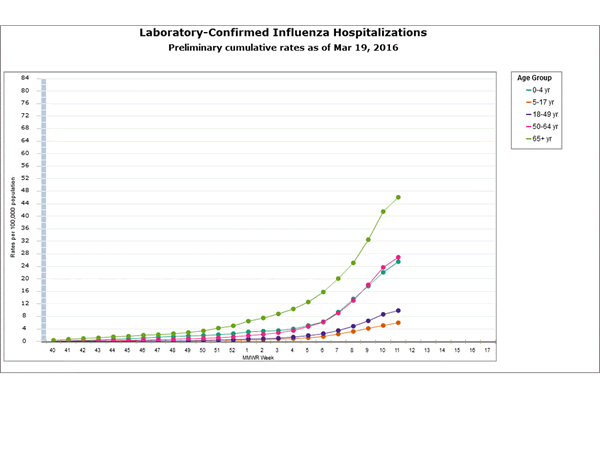
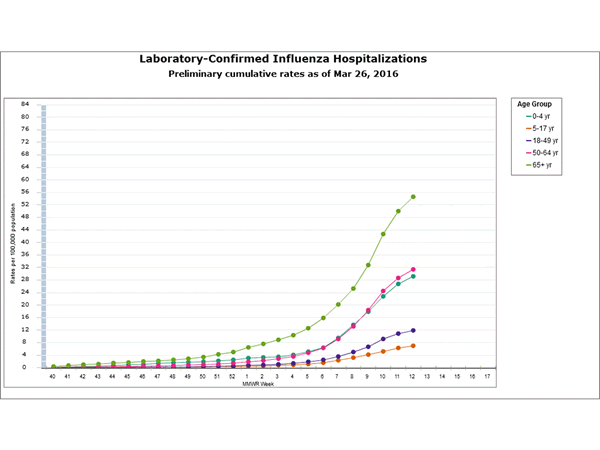
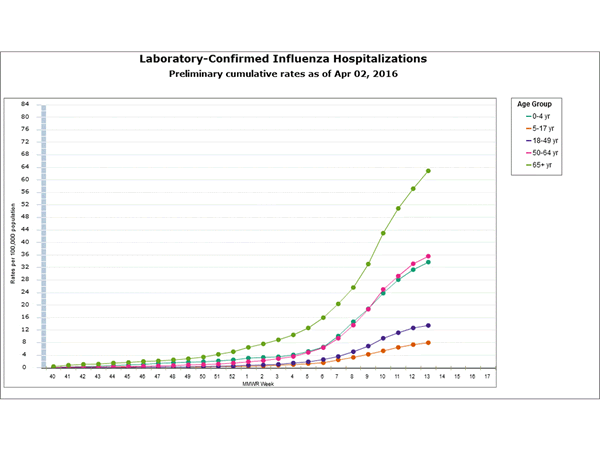
Influenza-Associated Hospitalizations:
The Influenza Hospitalization Surveillance Network (FluSurv-NET) conducts population-based surveillance for laboratory-confirmed influenza-related hospitalizations in children younger than 18 years of age (since the 2003-2004 influenza season) and adults (since the 2005-2006 influenza season).
The FluSurv-NET covers more than 70 counties in the 10 Emerging Infections Program (EIP) states (CA, CO, CT, GA, MD, MN, NM, NY, OR, and TN) and additional Influenza Hospitalization Surveillance Project (IHSP) states. The IHSP began during the 2009-2010 season to enhance surveillance during the 2009 H1N1 pandemic. IHSP sites included IA, ID, MI, OK and SD during the 2009-2010 season; ID, MI, OH, OK, RI, and UT during the 2010-2011 season; MI, OH, RI, and UT during the 2011-2012 season; IA, MI, OH, RI, and UT during the 2012-2013 season; and MI, OH, and UT during the 2013-2014, 2014-15 and 2015-16 seasons.
Data gathered are used to estimate age-specific hospitalization rates on a weekly basis, and describe characteristics of persons hospitalized with severe influenza illness. The rates provided are likely to be an underestimate as influenza-related hospitalizations can be missed, either because testing is not performed, or because cases may be attributed to other causes of pneumonia or other common influenza-related complications.
Between October 1, 2015 and February 13, 2016, 1,147 laboratory-confirmed influenza-associated hospitalizations were reported. The overall hospitalization rate was 4.1 per 100,000 population. The highest rate of hospitalization was among adults aged ≥65 years (12.7 per 100,000 population), followed by children aged 0-4 years (6.0 per 100,000 population) and adults aged 50-64 (5.2 per 100,000 population). Among all hospitalizations, 815 (71.1%) were associated with influenza A, 303 (26.4%) with influenza B, 20 (1.7%) with influenza A and B co-infection, and 9 (0.8%) had no virus type information. Among those with influenza A subtype information, 257 (86.0%) were A(H1N1)pdm09 and 42 (14.0%) were A(H3N2) virus.
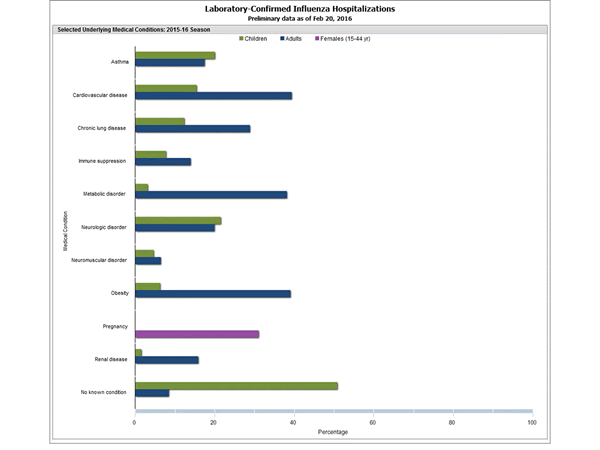
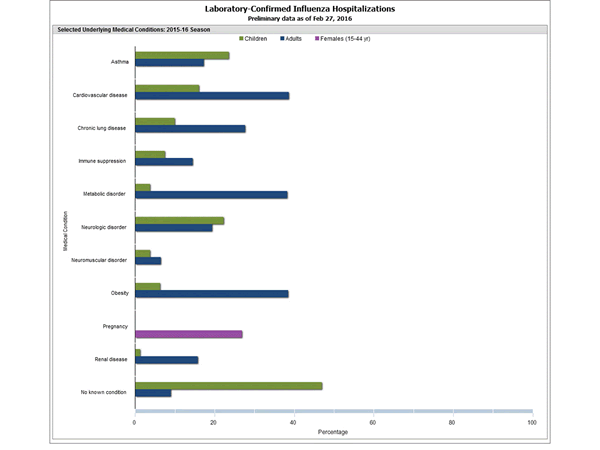
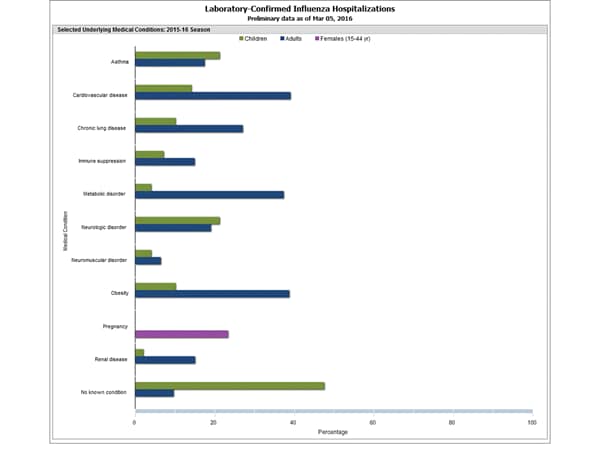
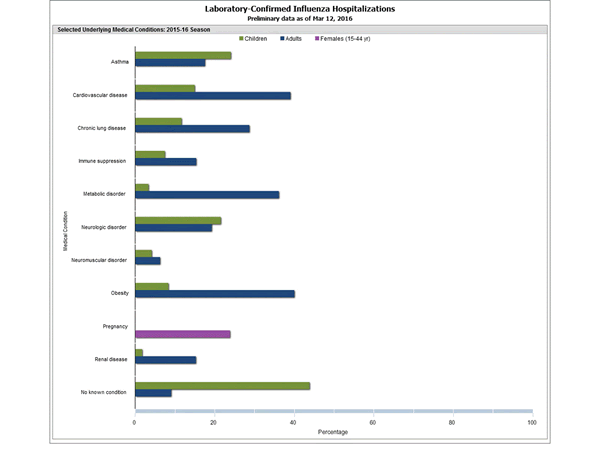
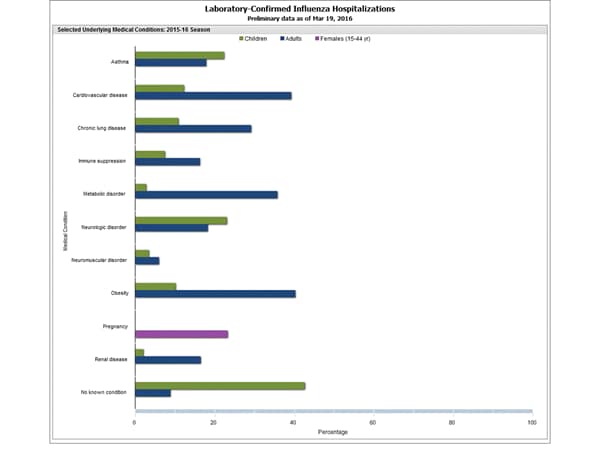
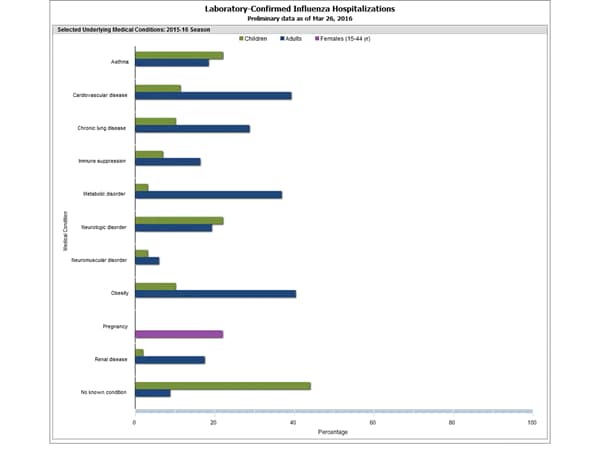
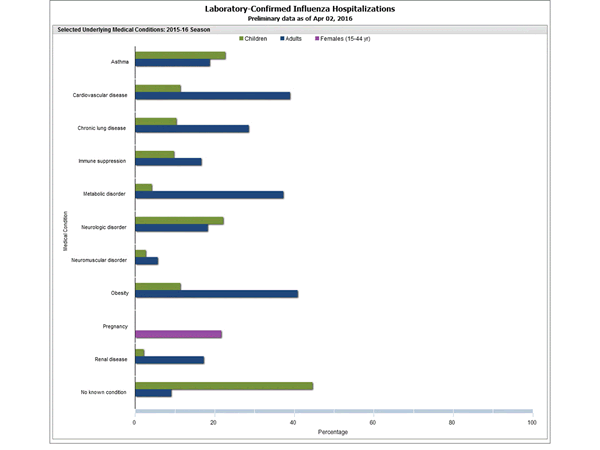
Clinical findings are preliminary and based on 352 (30.7%) cases with complete medical chart abstraction. The majority (91.5%) of hospitalized adults had at least one reported underlying medical condition; the most commonly reported were cardiovascular disease, metabolic disorders, and obesity. There were 54 hospitalized children with complete medical chart abstraction, 28 (51.9%) had no identified underlying medical conditions. The most commonly reported underlying medical conditions among pediatric patients were asthma, neurologic disorders and cardiovascular disease. Among the 34 hospitalized women of childbearing age (15-44 years), 9 were pregnant.
Additional FluSurv-NET data can be found at: http://gis.cdc.gov/GRASP/Fluview/FluHospRates.html and http://gis.cdc.gov/grasp/fluview/FluHospChars.html.
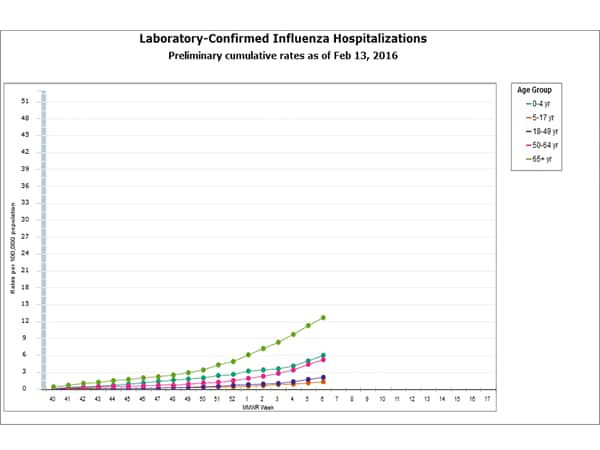
Data from the Influenza Hospitalization Surveillance Network (FluSurv-NET), a population-based surveillance for influenza related hospitalizations in children and adults in 13 U.S. states. Cumulative incidence rates are calculated using the National Center for Health Statistics’ (NCHS) population estimates for the counties included in the surveillance catchment area.
View Interactive Application | View Full Screen | View PowerPoint Presentation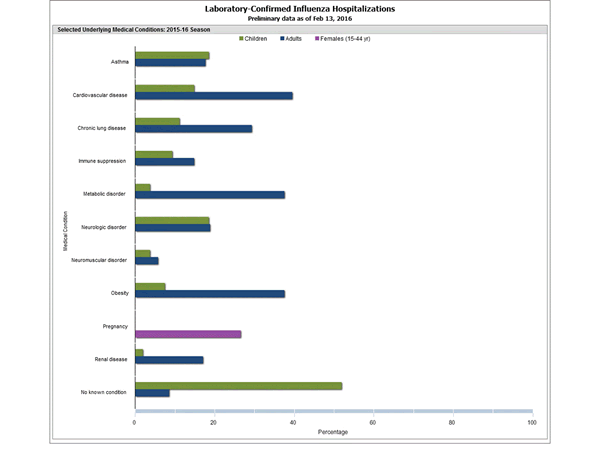
FluSurv-NET data are preliminary and displayed as they become available. Therefore, figures are based on varying denominators as some variables represent information that may require more time to be collected. Data are refreshed and updated weekly. Asthma includes a medical diagnosis of asthma or reactive airway disease; Cardiovascular diseases include conditions such as coronary heart disease, cardiac valve disorders, congestive heart failure, and pulmonary hypertension; does not include isolated hypertension; Chronic lung diseases include conditions such as chronic obstructive pulmonary disease, bronchiolitis obliterans, chronic aspiration pneumonia, and interstitial lung disease; Immune suppression includes conditions such as immunoglobulin deficiency, leukemia, lymphoma, HIV/AIDS, and individuals taking immunosuppressive medications; Metabolic disorders include conditions such as diabetes mellitus; Neurologic diseases include conditions such as seizure disorders, cerebral palsy, and cognitive dysfunction; Neuromuscular diseases include conditions such as multiple sclerosis and muscular dystrophy; Obesity was assigned if indicated in patient's medical chart or if body mass index (BMI) >30 kg/m2; Pregnancy percentage calculated using number of female cases aged between 15 and 44 years of age as the denominator; Renal diseases include conditions such as acute or chronic renal failure, nephrotic syndrome, glomerulonephritis, and impaired creatinine clearance; No known condition indicates that the case did not have any known high risk medical condition indicated in medical chart at the time of hospitalization.
View Interactive Application | View Full Screen | View PowerPoint Presentation
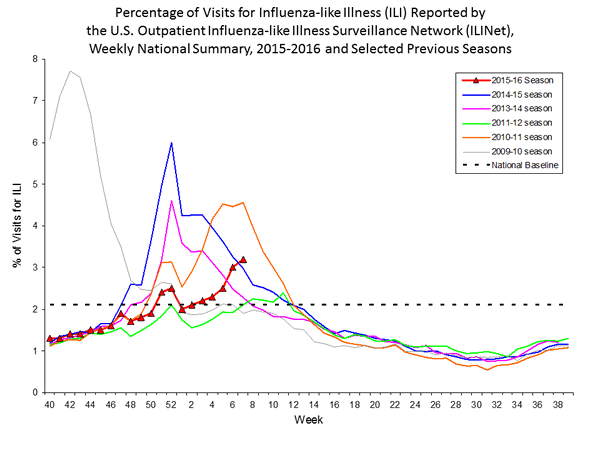
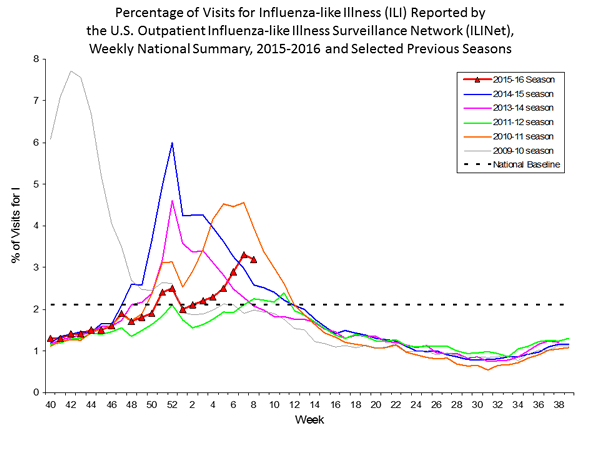
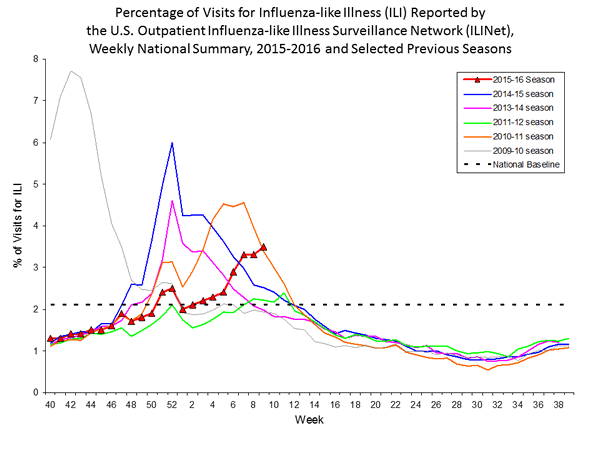
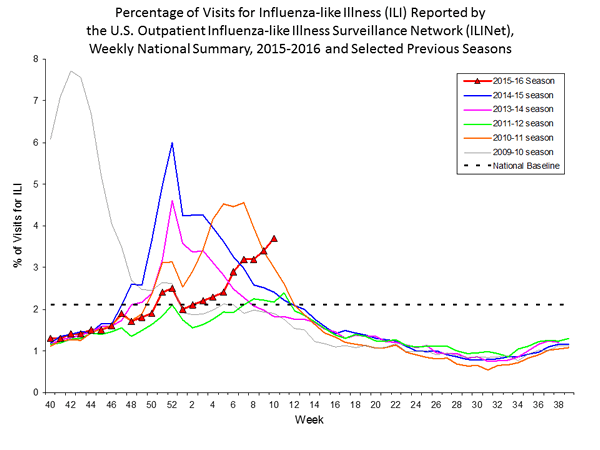
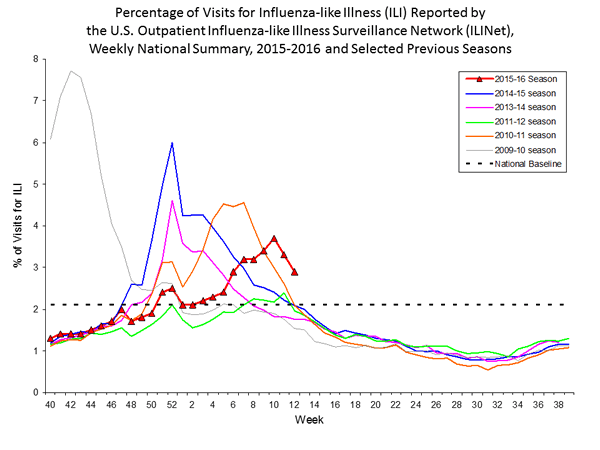
Outpatient Illness Surveillance:
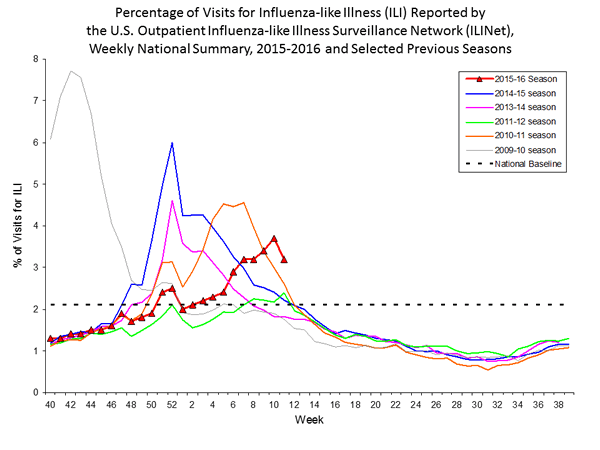
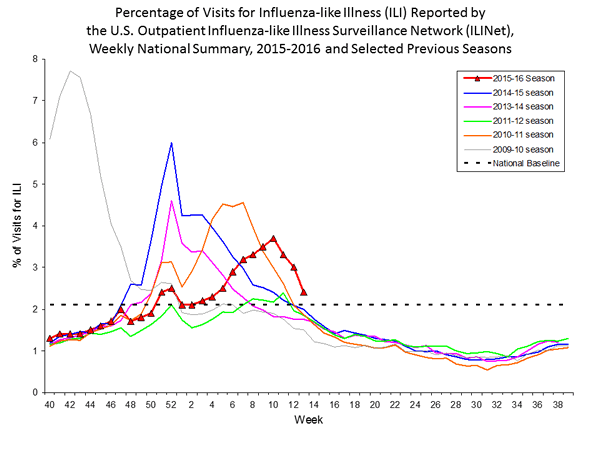
Nationwide during week 6, 3.1% of patient visits reported through the U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet) were due to influenza-like illness (ILI). This percentage is above the national baseline of 2.1%. (ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.)
The increase in the percentage of patient visits for ILI in weeks 51 and 52 (the weeks ending December 26, 2015 and January 2, 2016) may be influenced in part by a reduction in routine healthcare visits during the holidays, as has occurred in previous seasons.
Additional data are available at http://gis.cdc.gov/grasp/fluview/flu...dashboard.html.
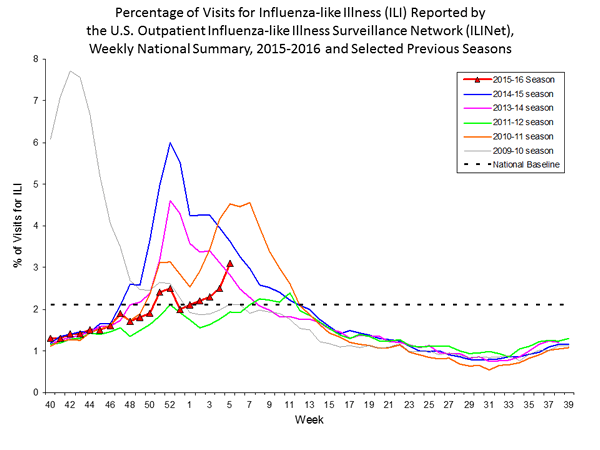
View National and Regional Level Graphs and Data | View Chart Data | View Full Screen | View PowerPoint Presentation On a regional level, the percentage of outpatient visits for ILI ranged from 1.4% to 5.1% during week 6. Nine regions (Regions 1, 2, 3, 4, 5, 6, 8, 9, and 10) reported a proportion of outpatient visits for ILI at or above their region-specific baseline levels.
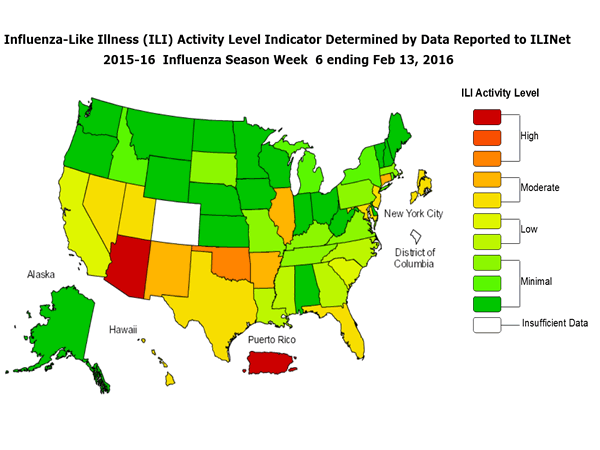
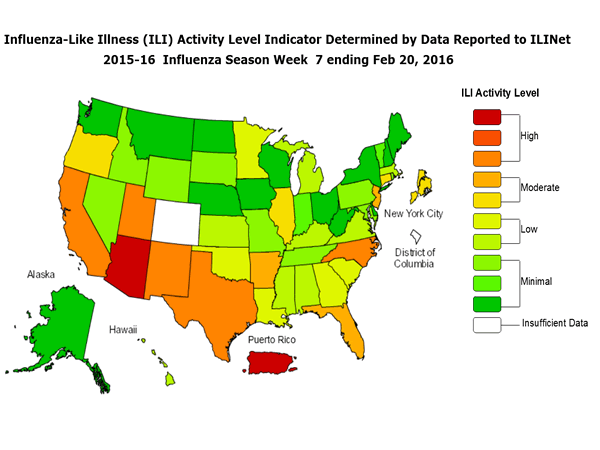
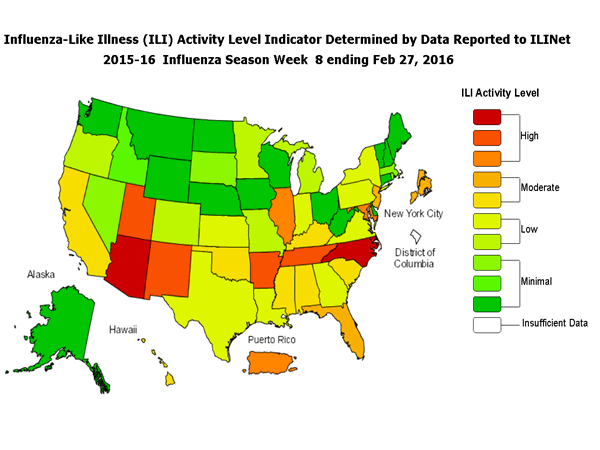
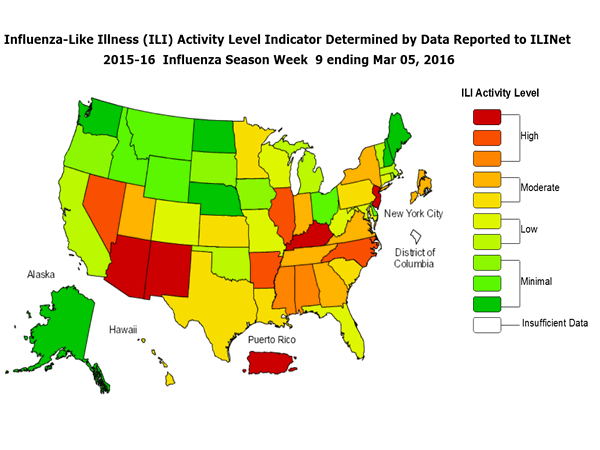
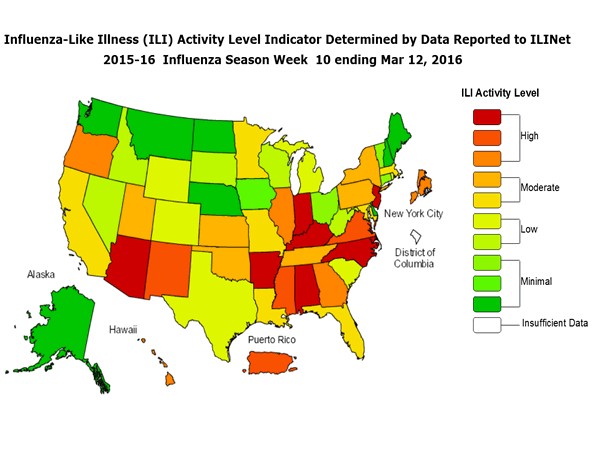
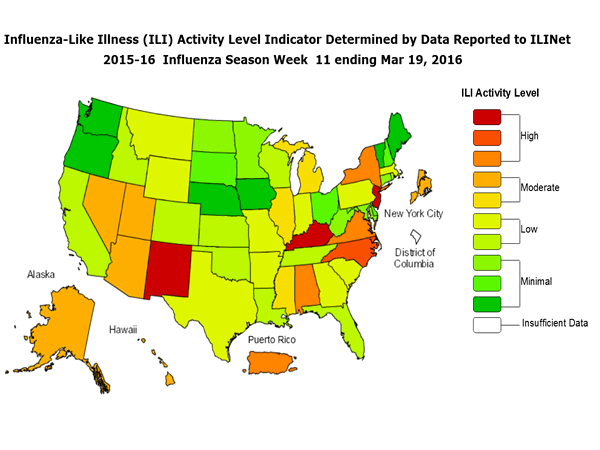
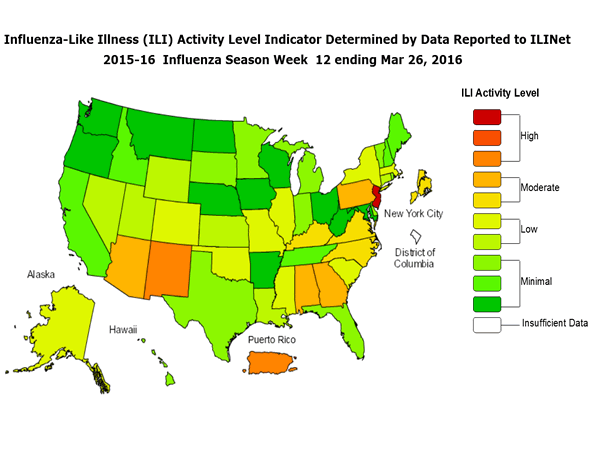
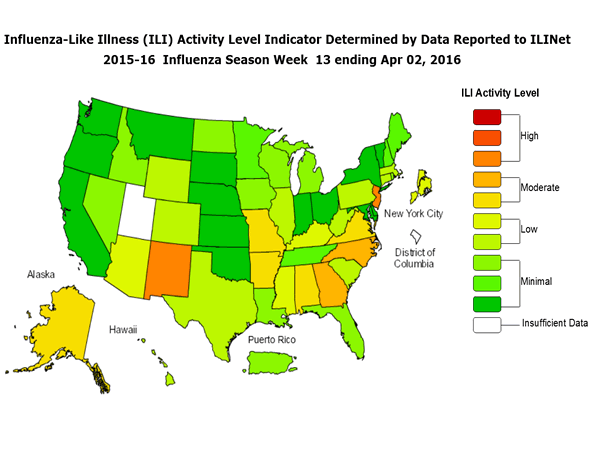
ILINet State Activity Indicator Map:
Data collected in ILINet are used to produce a measure of ILI activity* by state. Activity levels are based on the percent of outpatient visits in a state due to ILI and are compared to the average percent of ILI visits that occur during weeks with little or no influenza virus circulation. Activity levels range from minimal, which would correspond to ILI activity from outpatient clinics being below, or only slightly above, the average, to high, which would correspond to ILI activity from outpatient clinics being much higher than average.
During week 6, the following ILI activity levels were calculated:
Data collected in ILINet may disproportionally represent certain populations within a state, and therefore, may not accurately depict the full picture of influenza activity for the whole state.
Data displayed in this map are based on data collected in ILINet, whereas the State and Territorial flu activity map is based on reports from state and territorial epidemiologists. The data presented in this map is preliminary and may change as more data are received.
Differences in the data presented here by CDC and independently by some state health departments likely represent differing levels of data completeness with data presented by the state likely being the more complete.
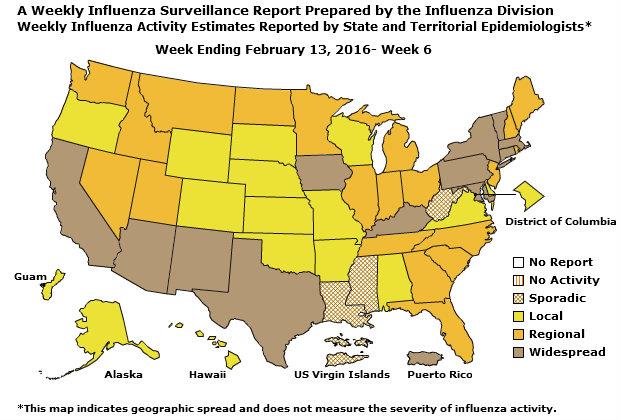
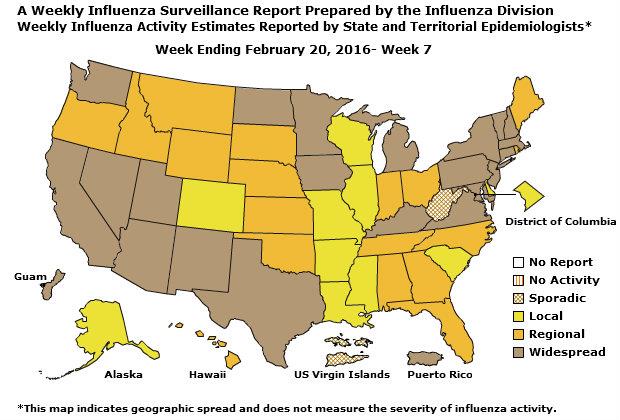
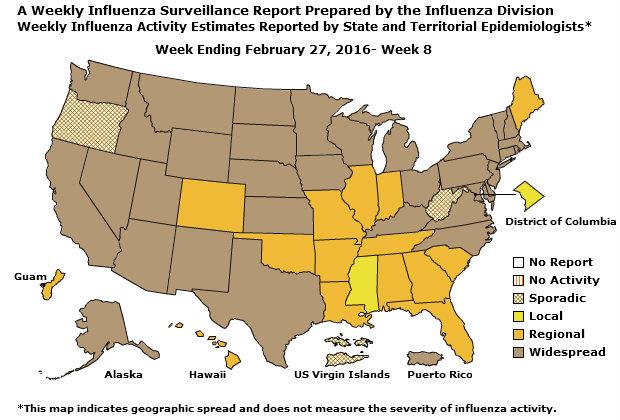
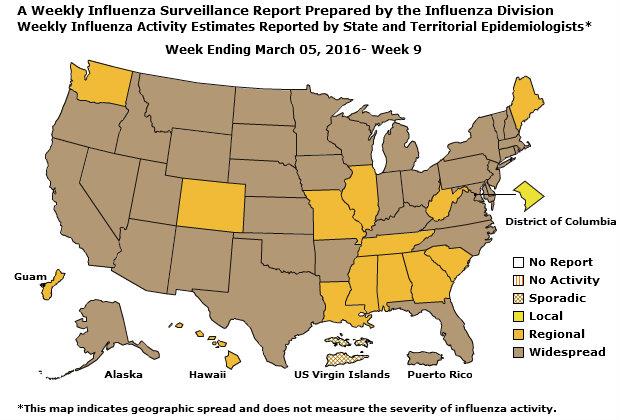
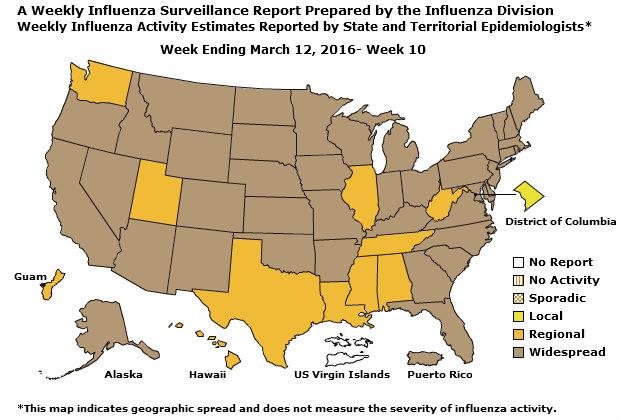
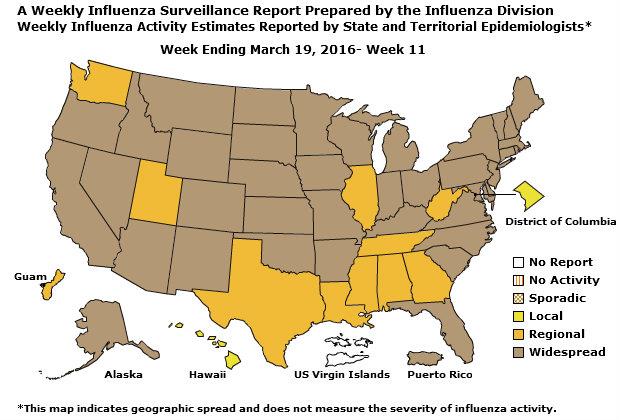
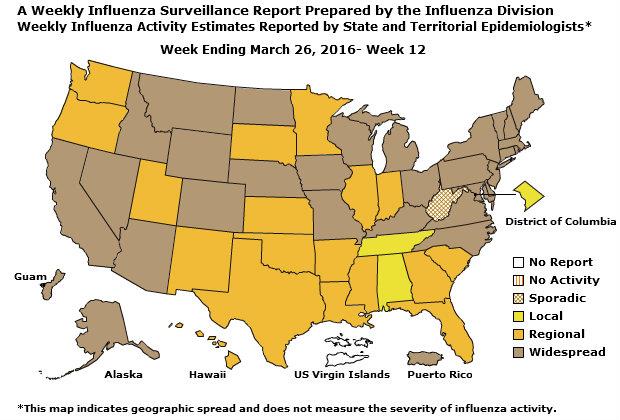
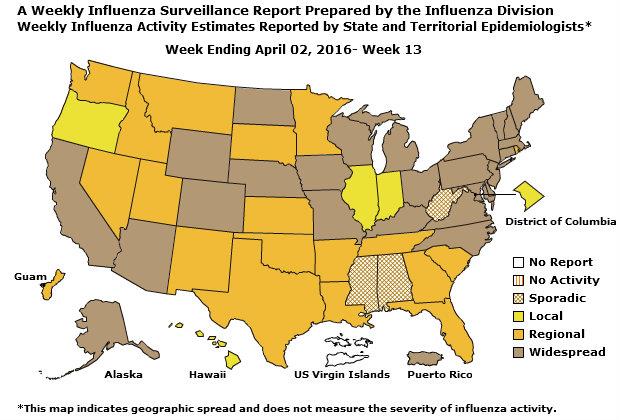
Geographic Spread of Influenza as Assessed by State and Territorial Epidemiologists
The influenza activity reported by state and territorial epidemiologists indicates geographic spread of influenza viruses, but does not measure the severity of influenza activity.
During week 6, the following influenza activity was reported: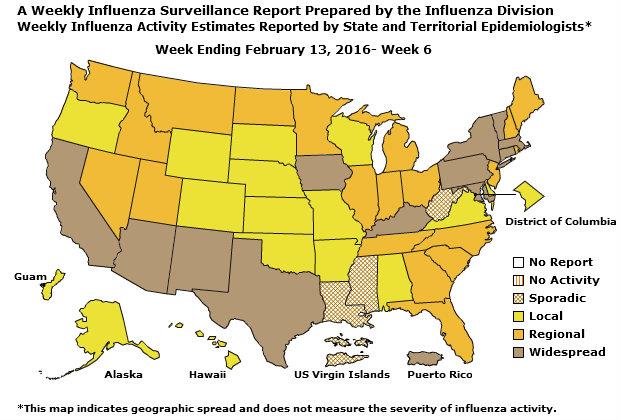
Additional National and International Influenza Surveillance Information
FluView Interactive: FluView includes enhanced web-based interactive applications that can provide dynamic visuals of the influenza data collected and analyzed by CDC. These FluView Interactive applications allow people to create customized, visual interpretations of influenza data, as well as make comparisons across flu seasons, regions, age groups and a variety of other demographics. To access these tools, visit http://www.cdc.gov/flu/weekly/fluviewinteractive.htm.
U.S. State and local influenza surveillance: Click on a jurisdiction below to access the latest local influenza information.
WHO Collaborating Centers for Influenza located in Australia, China, Japan, the United Kingdom, and the United States (CDC in Atlanta, Georgia).
Europe: For the most recent influenza surveillance information from Europe, please see WHO/Europe and the European Centre for Disease Prevention and Control at http://www.flunewseurope.org/
Public Health Agency of Canada: The most up-to-date influenza information from Canada is available at http://www.phac-aspc.gc.ca/fluwatch/
Public Health England: The most up-to-date influenza information from the United Kingdom is available at https://www.gov.uk/government/statistics/weekly-national-flu-reports
Any links provided to non-Federal organizations are provided solely as a service to our users. These links do not constitute an endorsement of these organizations or their programs by CDC or the Federal Government, and none should be inferred. CDC is not responsible for the content of the individual organization web pages found at these links.
An overview of the CDC influenza surveillance system, including methodology and detailed descriptions of each data component, is available at: http://www.cdc.gov/flu/weekly/overview.htm.
All data are preliminary and may change as more reports are received.
Synopsis:
During week 6 (February 7-13, 2016), influenza activity increased in the United States.
- Viral Surveillance: The most frequently identified influenza virus type reported by public health laboratories during week 6 was influenza A, with influenza A (H1N1)pdm09 viruses predominating. The percentage of respiratory specimens testing positive for influenza in clinical laboratories increased.
- Pneumonia and Influenza Mortality: The proportion of deaths attributed to pneumonia and influenza (P&I) was below their system-specific epidemic threshold in both the NCHS Mortality Surveillance System and the 122 Cities Mortality Reporting System.
- Influenza-associated Pediatric Deaths: Two influenza-associated pediatric deaths were reported.
- Influenza-associated Hospitalizations: A cumulative rate for the season of 4.1 laboratory-confirmed influenza-associated hospitalizations per 100,000 population was reported.
- Outpatient Illness Surveillance: The proportion of outpatient visits for influenza-like illness (ILI) was 3.1%, which is above the national baseline of 2.1%. Nine of 10 regions reported ILI at or above region-specific baseline levels. Puerto Rico and two states experienced high ILI activity; New York City and 11 states experienced moderate ILI activity; 6 states experienced low ILI activity; 30 states experienced minimal ILI activity; and the District of Columbia and one state had insufficient data.
- Geographic Spread of Influenza: The geographic spread of influenza in Puerto Rico and 12 states was reported as widespread; 20 states reported regional activity; the District of Columbia, Guam, and 15 states reported local activity; and the U.S. Virgin Islands and three states reported sporadic activity.
| Elevated | 15 of 53 | 12.0% | 2,459 | 980 | 120 | 178 | 531 | 482 | 13 |
| Elevated | 1 of 6 | 7.4% | 62 | 25 | 0 | 11 | 4 | 10 | 0 |
| Elevated | 3 of 4 | 8.0% | 159 | 101 | 2 | 14 | 5 | 17 | 1 |
| Elevated | 1 of 6 | 2.2% | 104 | 35 | 44 | 12 | 33 | 12 | 0 |
| Elevated | 1 of 8 | 14.0% | 200 | 88 | 13 | 8 | 6 | 93 | 4 |
| Elevated | 1 of 6 | 7.8% | 453 | 85 | 27 | 7 | 32 | 8 | 2 |
| Elevated | 4 of 5 | 4.7% | 51 | 71 | 5 | 7 | 11 | 33 | 1 |
| Normal | 0 of 4 | 3.3% | 102 | 31 | 1 | 5 | 9 | 4 | 0 |
| Elevated | 1 of 6 | 10.9% | 412 | 46 | 1 | 18 | 161 | 16 | 0 |
| Elevated | 3 of 4 | 13.8% | 728 | 420 | 21 | 74 | 172 | 209 | 4 |
| Elevated | 0 of 4 | 14.6% | 188 | 78 | 6 | 22 | 98 | 80 | 1 |
? Elevated means the % of visits for ILI is at or above the national or region-specific baseline
§ Includes all 50 states, New York City, the District of Columbia and Puerto Rico
? National data are for current week; regional data are for the most recent three weeks
U.S. Virologic Surveillance:
WHO and NREVSS collaborating laboratories, which include both public health and clinical laboratories located in all 50 states, Puerto Rico, and the District of Columbia, report to CDC the total number of respiratory specimens tested for influenza and the number positive for influenza by virus type. In addition, public health laboratories also report the influenza A subtype (H1 or H3) and influenza B lineage information of the viruses they test and the age or age group of the persons from whom the specimens were collected.
Additional data are available at http://gis.cdc.gov/grasp/fluview/flu...dashboard.html.
The results of tests performed by clinical laboratories during the current week are summarized below.
| 17,797 | 299,893 |
| 2,135 (12.0%) | 10,484 (3.5%) |
| 1,559 (73.0%) | 7,132 (68.0%) |
| 576 (27.0%) | 3,352 (32.0%) |
View National and Regional Level Graphs and Data | View Chart Data | View Full Screen | View PowerPoint Presentation The results of tests performed by public health laboratories, as well as the age group distribution of influenza positive tests, during the current week are summarized below.
| 1,531 | 29,151 |
| 580 | 4,750 |
| 423 (72.9%) | 3,559 (74.9%) |
| 361 (85.3%) | 2,459 (69.1%) |
| 51 (12.1%) | 980 (27.5%) |
| 11 (2.6%) | 120 (3.4%) |
| 157 (27.1%) | 1,191 (25.1%) |
| 63 (40.1%) | 531 (44.6%) |
| 27 (17.2%) | 178 (14.9%) |
| 67 (42.7%) | 482 (40.5%) |
View National and Regional Level Graphs and Data | View Chart Data | View Full Screen | View PowerPoint Presentation
View Chart Data | View Full Screen
View Chart Data |View Full Screen Influenza Virus Characterization:
CDC characterizes influenza viruses through one or more tests including genome sequencing, hemagglutination inhibition (HI) and/or neutralization assays. These data are used to compare how similar currently circulating influenza viruses are to the reference viruses used for developing influenza vaccines, and to monitor for changes in circulating influenza viruses. Historically, HI data have been used most commonly to assess the similarity between reference viruses and circulating viruses to suggest how well the vaccine may work until such time as vaccine effectiveness estimates are available. During the 2014–2015 season and to date, however, a portion of influenza A (H3N2) viruses do not yield sufficient hemagglutination titers for antigenic characterization by HI. For many of these viruses, CDC performs genetic characterization to determine the genetic group identity of those viruses. In this way, antigenic properties of these viruses can be inferred from viruses within the same genetic group that have been characterized antigenically.
CDC has characterized 532 influenza viruses [181 A (H1N1)pdm09, 228 A (H3N2), and 123 influenza B viruses] collected by U.S. laboratories since October 1, 2015.
Influenza A Virus [409]
- A (H1N1)pdm09 [181]: All 181 (100%) influenza A (H1N1)pdm09 viruses were antigenically characterized as A/California/7/2009-like, the influenza A (H1N1) component of the 2015-2016 Northern Hemisphere vaccine.
- A (H3N2) [228]: All 228 H3N2 viruses were genetically sequenced and all viruses belonged to genetic groups for which a majority of viruses antigenically characterized were similar to the cell-propagated A/Switzerland/9715293/2013, the influenza A (H3N2) reference virus representing the 2015-2016 Northern Hemisphere vaccine component.
- A subset of 107 H3N2 viruses also were antigenically characterized; 100 of 107 (93.5%) H3N2 viruses were A/Switzerland/9715293/2013-like by HI testing or neutralization testing.
- Yamagata Lineage [88]: All 88 (100%) B/Yamagata-lineage viruses were antigenically characterized as B/Phuket/3073/2013-like, which is included as an influenza B component of the 2015-2016 Northern Hemisphere trivalent and quadrivalent influenza vaccines.
- Victoria Lineage [35]: All 35 (100%) B/Victoria-lineage viruses were antigenically characterized as B/Brisbane/60/2008-like, which is included as an influenza B component of the 2015-2016 Northern Hemisphere quadrivalent influenza vaccines.
Testing of influenza A(H1N1)pdm09, A(H3N2), and influenza B virus isolates for resistance to neuraminidase inhibitors (oseltamivir, zanamivir, and peramivir) is performed at CDC using a functional assay. Additional A(H1N1)pdm09 and A(H3N2) clinical samples are tested for mutations of the virus known to confer oseltamivir resistance. The data summarized below combine the results of both testing methods. These samples are routinely obtained for surveillance purposes rather than for diagnostic testing of patients suspected to be infected with antiviral-resistant virus.
High levels of resistance to the adamantanes (amantadine and rimantadine) persist among A(H1N1)pdm09 and A(H3N2) viruses (the adamantanes are not effective against influenza B viruses). Therefore, data from adamantane resistance testing are not presented below.
| 330 | 2 (0.6) | 252 | 0 (0.0) | 330 | 2 (0.6) |
| 261 | 0 (0.0) | 261 | 0 (0.0) | 247 | 0 (0.0) |
| 202 | 0 (0.0) | 202 | 0 (0.0) | 202 | 0 (0.0) |
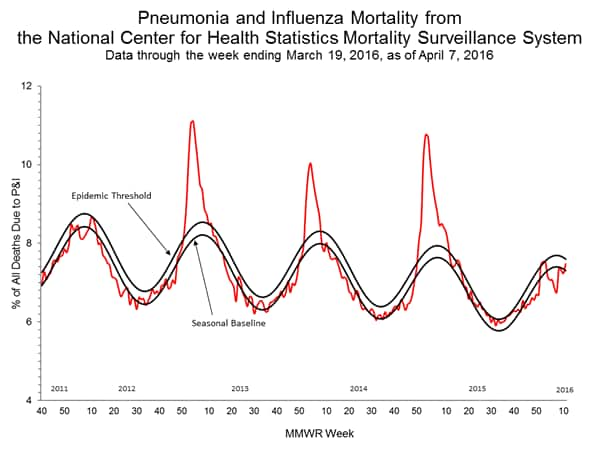
Pneumonia and Influenza (P&I) Mortality Surveillance:
Rapid tracking of pneumonia and influenza-associated deaths is done through two systems, the National Center for Health Statistics (NCHS) Mortality Surveillance System and the 122 Cities Mortality Reporting System. NCHS mortality surveillance data are presented by the week the death occurred and P&I percentages are released two weeks after the week of death to allow for collection of enough data to produce a stable P&I percentage. Users of the data should not expect the two systems to produce the same percentages, and the percent P&I deaths from each system should be compared to the corresponding system-specific baselines and thresholds.
NCHS Mortality Surveillance Data:
Based on NCHS mortality surveillance data available on February 18, 2016, 6.5% of the deaths occurring during the week ending January 30, 2016 (week 4) were due to P&I. This percentage is below the epidemic threshold of 7.6% for week 4.
Region and state-specific data are available at http://www.cdc.gov/flu/weekly/nchs.htm.
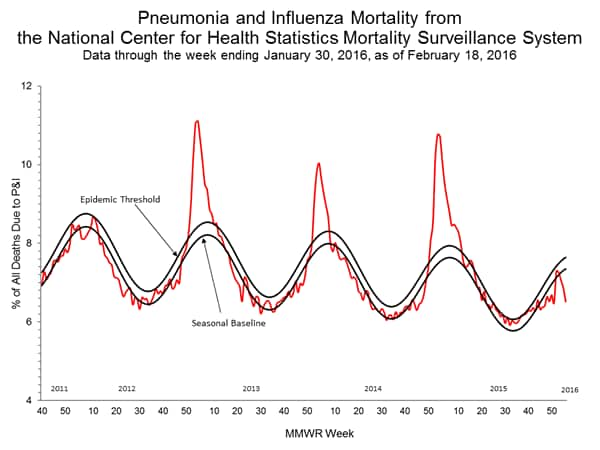
View Regional and State Level Data | View Chart Data | View Full Screen | View PowerPoint Presentation 122 Cities Mortality Reporting System:
During week 6, 6.9% of all deaths reported through the 122 Cities Mortality Reporting System were due to P&I. This percentage was below the epidemic threshold of 7.3% for week 6.
View Full Screen | View PowerPoint Presentation
Influenza-Associated Pediatric Mortality:
Two influenza-associated pediatric deaths were reported to CDC during week 6. One death was associated with an influenza A (H1N1)pdm09 virus and occurred during week 2 (the week ending January 16, 2016). One death was associated with an influenza virus for which the type was not determined and occurred during week 6 (the week ending February 13, 2016).
A total of 13 influenza-associated pediatric deaths have been reported during the 2015-2016 season from Puerto Rico [1], Chicago [1], and eight states (Arizona [1], California [2], Florida [3], Louisiana [1], Michigan [1], Nevada [1], Tennessee [1], and Washington [1]).
Additional data can be found at: http://gis.cdc.gov/GRASP/Fluview/PedFluDeath.html.
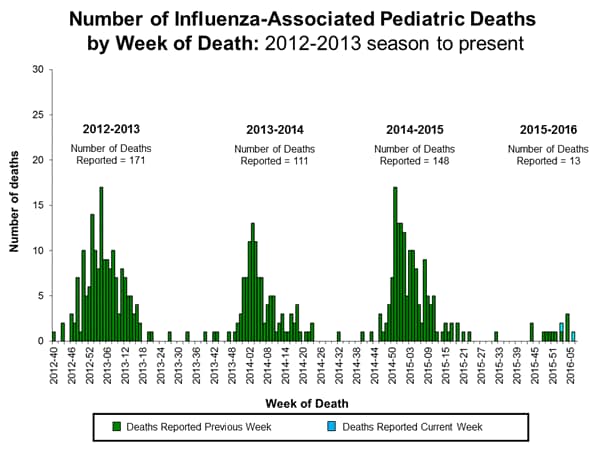
View Interactive Application | View Full Screen | View PowerPoint Presentation
Influenza-Associated Hospitalizations:
The Influenza Hospitalization Surveillance Network (FluSurv-NET) conducts population-based surveillance for laboratory-confirmed influenza-related hospitalizations in children younger than 18 years of age (since the 2003-2004 influenza season) and adults (since the 2005-2006 influenza season).
The FluSurv-NET covers more than 70 counties in the 10 Emerging Infections Program (EIP) states (CA, CO, CT, GA, MD, MN, NM, NY, OR, and TN) and additional Influenza Hospitalization Surveillance Project (IHSP) states. The IHSP began during the 2009-2010 season to enhance surveillance during the 2009 H1N1 pandemic. IHSP sites included IA, ID, MI, OK and SD during the 2009-2010 season; ID, MI, OH, OK, RI, and UT during the 2010-2011 season; MI, OH, RI, and UT during the 2011-2012 season; IA, MI, OH, RI, and UT during the 2012-2013 season; and MI, OH, and UT during the 2013-2014, 2014-15 and 2015-16 seasons.
Data gathered are used to estimate age-specific hospitalization rates on a weekly basis, and describe characteristics of persons hospitalized with severe influenza illness. The rates provided are likely to be an underestimate as influenza-related hospitalizations can be missed, either because testing is not performed, or because cases may be attributed to other causes of pneumonia or other common influenza-related complications.
Between October 1, 2015 and February 13, 2016, 1,147 laboratory-confirmed influenza-associated hospitalizations were reported. The overall hospitalization rate was 4.1 per 100,000 population. The highest rate of hospitalization was among adults aged ≥65 years (12.7 per 100,000 population), followed by children aged 0-4 years (6.0 per 100,000 population) and adults aged 50-64 (5.2 per 100,000 population). Among all hospitalizations, 815 (71.1%) were associated with influenza A, 303 (26.4%) with influenza B, 20 (1.7%) with influenza A and B co-infection, and 9 (0.8%) had no virus type information. Among those with influenza A subtype information, 257 (86.0%) were A(H1N1)pdm09 and 42 (14.0%) were A(H3N2) virus.
Clinical findings are preliminary and based on 352 (30.7%) cases with complete medical chart abstraction. The majority (91.5%) of hospitalized adults had at least one reported underlying medical condition; the most commonly reported were cardiovascular disease, metabolic disorders, and obesity. There were 54 hospitalized children with complete medical chart abstraction, 28 (51.9%) had no identified underlying medical conditions. The most commonly reported underlying medical conditions among pediatric patients were asthma, neurologic disorders and cardiovascular disease. Among the 34 hospitalized women of childbearing age (15-44 years), 9 were pregnant.
Additional FluSurv-NET data can be found at: http://gis.cdc.gov/GRASP/Fluview/FluHospRates.html and http://gis.cdc.gov/grasp/fluview/FluHospChars.html.
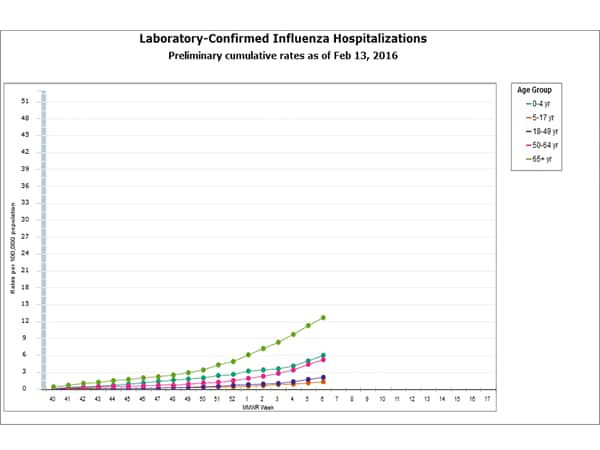
Data from the Influenza Hospitalization Surveillance Network (FluSurv-NET), a population-based surveillance for influenza related hospitalizations in children and adults in 13 U.S. states. Cumulative incidence rates are calculated using the National Center for Health Statistics’ (NCHS) population estimates for the counties included in the surveillance catchment area.
View Interactive Application | View Full Screen | View PowerPoint Presentation
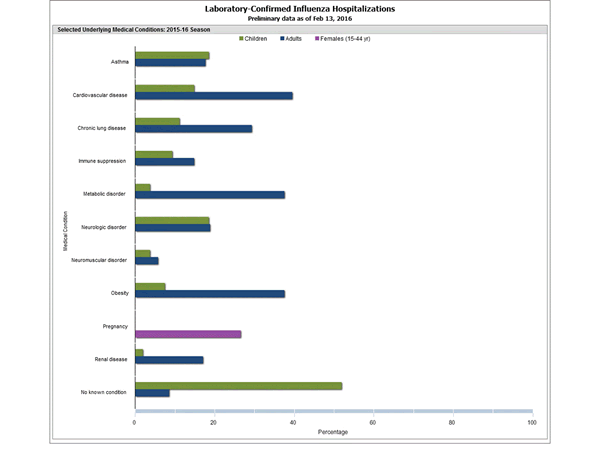
FluSurv-NET data are preliminary and displayed as they become available. Therefore, figures are based on varying denominators as some variables represent information that may require more time to be collected. Data are refreshed and updated weekly. Asthma includes a medical diagnosis of asthma or reactive airway disease; Cardiovascular diseases include conditions such as coronary heart disease, cardiac valve disorders, congestive heart failure, and pulmonary hypertension; does not include isolated hypertension; Chronic lung diseases include conditions such as chronic obstructive pulmonary disease, bronchiolitis obliterans, chronic aspiration pneumonia, and interstitial lung disease; Immune suppression includes conditions such as immunoglobulin deficiency, leukemia, lymphoma, HIV/AIDS, and individuals taking immunosuppressive medications; Metabolic disorders include conditions such as diabetes mellitus; Neurologic diseases include conditions such as seizure disorders, cerebral palsy, and cognitive dysfunction; Neuromuscular diseases include conditions such as multiple sclerosis and muscular dystrophy; Obesity was assigned if indicated in patient's medical chart or if body mass index (BMI) >30 kg/m2; Pregnancy percentage calculated using number of female cases aged between 15 and 44 years of age as the denominator; Renal diseases include conditions such as acute or chronic renal failure, nephrotic syndrome, glomerulonephritis, and impaired creatinine clearance; No known condition indicates that the case did not have any known high risk medical condition indicated in medical chart at the time of hospitalization.
View Interactive Application | View Full Screen | View PowerPoint Presentation
Outpatient Illness Surveillance:
Nationwide during week 6, 3.1% of patient visits reported through the U.S. Outpatient Influenza-like Illness Surveillance Network (ILINet) were due to influenza-like illness (ILI). This percentage is above the national baseline of 2.1%. (ILI is defined as fever (temperature of 100°F [37.8°C] or greater) and cough and/or sore throat.)
The increase in the percentage of patient visits for ILI in weeks 51 and 52 (the weeks ending December 26, 2015 and January 2, 2016) may be influenced in part by a reduction in routine healthcare visits during the holidays, as has occurred in previous seasons.
Additional data are available at http://gis.cdc.gov/grasp/fluview/flu...dashboard.html.
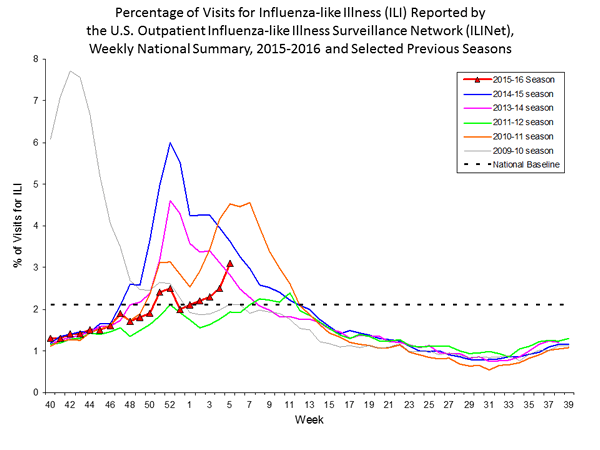
View National and Regional Level Graphs and Data | View Chart Data | View Full Screen | View PowerPoint Presentation On a regional level, the percentage of outpatient visits for ILI ranged from 1.4% to 5.1% during week 6. Nine regions (Regions 1, 2, 3, 4, 5, 6, 8, 9, and 10) reported a proportion of outpatient visits for ILI at or above their region-specific baseline levels.
ILINet State Activity Indicator Map:
Data collected in ILINet are used to produce a measure of ILI activity* by state. Activity levels are based on the percent of outpatient visits in a state due to ILI and are compared to the average percent of ILI visits that occur during weeks with little or no influenza virus circulation. Activity levels range from minimal, which would correspond to ILI activity from outpatient clinics being below, or only slightly above, the average, to high, which would correspond to ILI activity from outpatient clinics being much higher than average.
During week 6, the following ILI activity levels were calculated:
- Puerto Rico and two states (Arizona and Oklahoma) experienced high ILI activity.
- New York City and 11 states (Arkansas, Connecticut, Florida, Hawaii, Illinois, Maryland, Nevada, New Jersey, New Mexico, Texas, and Utah) experienced moderate ILI activity.
- Six states (California, Georgia, Louisiana, Mississippi, North Carolina, and South Carolina) experienced low ILI activity.
- 30 states (Alabama, Alaska, Delaware, Idaho, Indiana, Iowa, Kansas, Kentucky, Maine, Massachusetts, Michigan, Minnesota, Missouri, Montana, Nebraska, New Hampshire, New York, North Dakota, Ohio, Oregon, Pennsylvania, Rhode Island, South Dakota, Tennessee, Vermont, Virginia, Washington, West Virginia, Wisconsin, and Wyoming) experienced minimal ILI activity.
- Data were insufficient to calculate an ILI activity level from the District of Columbia and one state (Colorado).
Click on map to launch interactive tool
*This map uses the proportion of outpatient visits to health care providers for ILI to measure the ILI activity level within a state. It does not, however, measure the extent of geographic spread of flu within a state. Therefore, outbreaks occurring in a single city could cause the state to display high activity levels.Data collected in ILINet may disproportionally represent certain populations within a state, and therefore, may not accurately depict the full picture of influenza activity for the whole state.
Data displayed in this map are based on data collected in ILINet, whereas the State and Territorial flu activity map is based on reports from state and territorial epidemiologists. The data presented in this map is preliminary and may change as more data are received.
Differences in the data presented here by CDC and independently by some state health departments likely represent differing levels of data completeness with data presented by the state likely being the more complete.
Geographic Spread of Influenza as Assessed by State and Territorial Epidemiologists
The influenza activity reported by state and territorial epidemiologists indicates geographic spread of influenza viruses, but does not measure the severity of influenza activity.
During week 6, the following influenza activity was reported:
- Widespread influenza activity was reported by Puerto Rico and 12 states (Arizona, California, Connecticut, Iowa, Kentucky, Maryland, Massachusetts, New Mexico, New York, Pennsylvania, Texas, and Vermont).
- Regional influenza activity was reported by 20 states (Florida, Georgia, Idaho, Illinois, Indiana, Maine, Michigan, Minnesota, Montana, Nevada, New Hampshire, New Jersey, North Carolina, North Dakota, Ohio, Rhode Island, South Carolina, Tennessee, Utah, and Washington).
- Local influenza activity was reported by the District of Columbia, Guam and 15 states (Alabama, Alaska, Arkansas, Colorado, Delaware, Hawaii, Kansas, Missouri, Nebraska, Oklahoma, Oregon, South Dakota, Virginia, Wisconsin, and Wyoming).
- Sporadic influenza activity was reported by the U.S. Virgin Islands and three states (Louisiana, Mississippi, and West Virginia).
Additional National and International Influenza Surveillance Information
FluView Interactive: FluView includes enhanced web-based interactive applications that can provide dynamic visuals of the influenza data collected and analyzed by CDC. These FluView Interactive applications allow people to create customized, visual interpretations of influenza data, as well as make comparisons across flu seasons, regions, age groups and a variety of other demographics. To access these tools, visit http://www.cdc.gov/flu/weekly/fluviewinteractive.htm.
U.S. State and local influenza surveillance: Click on a jurisdiction below to access the latest local influenza information.
World Health Organization: Additional influenza surveillance information from participating WHO member nations is available through FluNet and the Global Epidemiology Reports.
WHO Collaborating Centers for Influenza located in Australia, China, Japan, the United Kingdom, and the United States (CDC in Atlanta, Georgia).
Europe: For the most recent influenza surveillance information from Europe, please see WHO/Europe and the European Centre for Disease Prevention and Control at http://www.flunewseurope.org/
Public Health Agency of Canada: The most up-to-date influenza information from Canada is available at http://www.phac-aspc.gc.ca/fluwatch/
Public Health England: The most up-to-date influenza information from the United Kingdom is available at https://www.gov.uk/government/statistics/weekly-national-flu-reports
Any links provided to non-Federal organizations are provided solely as a service to our users. These links do not constitute an endorsement of these organizations or their programs by CDC or the Federal Government, and none should be inferred. CDC is not responsible for the content of the individual organization web pages found at these links.
An overview of the CDC influenza surveillance system, including methodology and detailed descriptions of each data component, is available at: http://www.cdc.gov/flu/weekly/overview.htm.

Comment