Neeja Bakshi
@NeejaB
A very long - Long COVID thread. Our Long COVID program has been open 10 months now. I've seen over 150 patients in that time, with new referrals booking well into February 2023.
10:56 PM · Oct 27, 2022·Twitter for Android
1,564
Retweets
159
Quote Tweets
4,486
Likes

Tweet your reply
Reply

Neeja Bakshi
@NeejaB
·
13h
Replying to
@NeejaB
I've had to stop accepting other internal medicine referrals, just so I can keep up with the demand, the follow ups, the downstream effect.
3
39
638

Neeja Bakshi
@NeejaB
·
13h
What I've learned... There are definite patterns. Dysautonomia/POTS. Cognitive dysfunction and brain fog. PEM (post exertional malaise). Unexplained rashes. Muscles feeling like cement. Migraines. Chest pain. So much chest pain. Shortness of breath.
16
195
1,265

Neeja Bakshi
@NeejaB
·
13h
Who I've seen.... Humans of all ages. 21 through 87. All demographics. Previously healthy. Previously not healthy. Teachers and healthcare workers. So many teachers and healthcare workers. Athletes. Non athletes. It's non-discrimnatory.
3
160
1,242

Neeja Bakshi
@NeejaB
·
13h
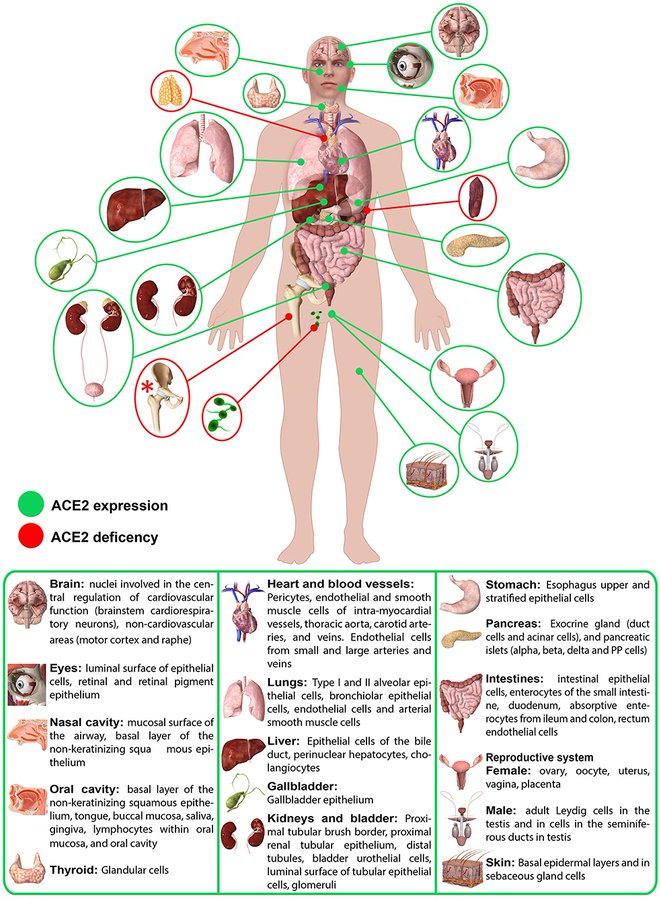
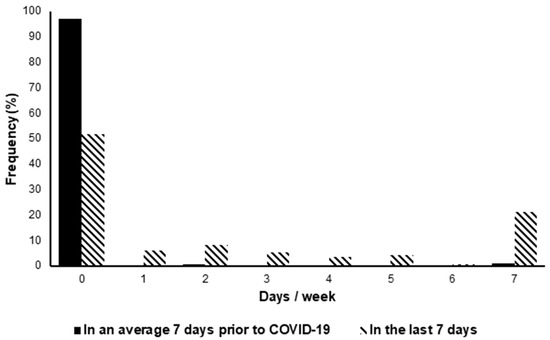
How my clinical process has evolved.... Pre-appt screening tests, quality of life scores, functional assessment scores. During appointment visual aids to help understand possible pathophysiology.
2
33
645

Neeja Bakshi
@NeejaB
·
13h
Comprehensive educational documentation with personalized recommendations for each patient as info is often overwhelming, esp with brain fog. Treatment aimed at both "Band-Aid toolbox" to help quality of life and "Root cause" looking at immunomodulation, anti-inflammation.
3
45
724

Neeja Bakshi
@NeejaB
·
13h
Nursing and physician check ins. Regularly. Reflective listening, validation, and commiseration. Continuously reading, searching, hoping to find next breakthrough or tool that can be used.
3
35
676

Neeja Bakshi
@NeejaB
·
13h
Barriers I've discovered - insurance. Insurance. Insurance. Insurance. Pages and pages of forms, minimizing my judgement, experience and clinical knowledge.
4
139140
1,251

Neeja Bakshi
@NeejaB
·
13h

Neeja Bakshi
@NeejaB
·
13h
Fighting tooth and nail to have claim adjusters understand that "pushing through" and excessive functional assessments for the patient is contraindicated in patients with long COVID and ME/CFS.
2
126
1,120

Neeja Bakshi
@NeejaB
·
13h
And through all of this, trying to manage my own long COVID experience. Which has required pacing, reinvention of my chart note template to help cue the next question I was supposed to ask.
1
40
897

Neeja Bakshi
@NeejaB
·
13h
I let my patients know at the beginning of their long covid assessment, that the 90 minutes allotted is not only for them, but for me... As I will undoubtedly require the time and space to fully stay on task.
1
36
806

Neeja Bakshi
@NeejaB
·
12h
The 15 minute buffers I have to place throughout my day to regain the line of questioning and follow through needed that comes with each individual's Long COVID story.
2
28
671

Neeja Bakshi
@NeejaB
·
12h
10 months in, some of my patients have been able to be discharged, feeling almost close to pre -COVID health. Some have gotten COVID again, which worsens their symptoms and we start everything from scratch.
3
78
820

Neeja Bakshi
@NeejaB
·
13h
But the vast majority of Long COVID patients are in this purgatory. Not knowing which way their life is going to go. Is this the best it's going to be? Am I one illness away from going back to where I started? Will I be able to work again? Will I feel normal again?
4
156
1,038

Neeja Bakshi
@NeejaB
·
13h
After 2.5 years, we have only begun to scratch the surface of Long COVID, and understand its impact on individuals. I fear we will continue to underestimate its impact on our province, our nation and truly the world. #LongCovid
34
223
1,466

Neeja Bakshi
@NeejaB
·
3h
Edited: thank you for the shares and the comments. Couple of common questions came up, I'll try to address, with the disclaimer that this is not medical advice, & while experiential medicine is important, I am very clear with my patients about risk vs benefit in any intervention.
1
7
172

Neeja Bakshi
@NeejaB
·
3h
1. What treatments am I recommending? If dysautonomia/POTS- common known tx: fluids, electrolytes, beta blockers, ivabradine (the latter often comes with cost / coverage barrier). Fatigue/inflammatory symptoms: antihistamines (Blexten, rupall); LDN (low dose naltrexone)
4
22
208

Neeja Bakshi
@NeejaB
·
3h
Other treatments usually based on symptoms - vitamin deficiency replacement, mood support (ADHD, depression), inhalers, anti-inflammatories, and much much more. Non pharmacological - rehabilitation (with the right team that understands CFS), acupuncture, counseling / CBT.
5
14
170

Neeja Bakshi
@NeejaB
·
3h
2. Vax vs unvaxxed - remember, this is a small sample size. Purely anecdotal. Those that got COVID in 2020 prior to vaccine being available (in my cohort) show far more debilitating and severe long COVID than those with even one dose. Vaccinated individuals can still get LC.
2
28
268

Neeja Bakshi
@NeejaB
·
3h
Unvaxxed appears to have worse symptomatology (again. Only in what I am seeing, this is not the same as a robust study that will be needed in general for LC).
1
13
189

Neeja Bakshi
@NeejaB
·
3h
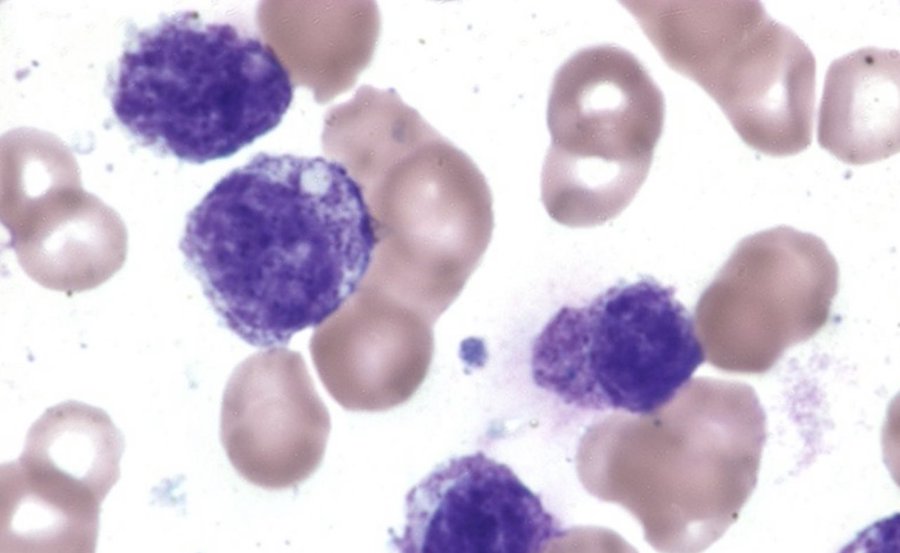
3. This sounds like many other autoimmune, post-infectious syndromes that many suffer from: I agree. I am hopeful that that attention being given to LC, the subsequent research and treatment guidelines - will help a far larger population of patients who have been ill for so long.














Comment