Statement – 36 million people across the European Region may have developed long COVID over the first 3 years of the pandemic
Statement by Dr Hans Henri P. Kluge, WHO Regional Director for Europe to the press on COVID-19, extreme heat and mpox
27 June 2023 Statement
...
This summer will be the first in more than 3 years that many of us will enjoy without the looming threat of COVID-19.
Whilst it may not be a global public health emergency, COVID-19 has not gone away.
Close to 1000 new COVID-19 deaths continue to occur across the Region every week, and this is an underestimate due to a drop in countries regularly reporting COVID-19 deaths to WHO.
And it continues to disproportionately affect the weakest and the most vulnerable.
COVID-19 exploited an epidemic of diseases, including cancers, cardiovascular disease, diabetes, and chronic lung illnesses, which account for 75% of mortality in our region today. Those with such underlying conditions were, and still are, far more vulnerable to severe forms of COVID-19.
Yet simple solutions can help reduce the burden of these so-called noncommunicable diseases, and fight the next pandemic when it arrives. Those of us with the means and opportunity can, for example, undertake 25 minutes of moderate exercise a day, quit smoking, moderate alcohol consumption and limit salt intake.
Long COVID remains a complex condition we still know very little about.
According to estimates from our collaborating centre, the Institute for Health Metrics and Evaluation at the University of Washington in Seattle, nearly 36 million people across the WHO European Region may have experienced long COVID in the first 3 years of the pandemic.
That’s approximately 1 in 30 Europeans over the past 3 years.
That’s 1 in 30 who may still be finding it hard to return to normal life.
1 in 30 who could be suffering in silence, left behind as others move on from COVID-19.
We are listening to the calls from long COVID patients and support groups, and raising awareness of their plight, but clearly much more needs to be done to understand it.
Long COVID remains a glaring blind spot in our knowledge, that urgently needs to be filled.
Unless we develop comprehensive diagnostics and treatment for long COVID, we will never truly recover from the pandemic. We are encouraging more research to be undertaken and urging those eligible for COVID-19 vaccination to be vaccinated. This under-recognized condition should be taken seriously, across the health and social sectors, and we should ensure ample care is available for patients.
Ultimately, the best way to avoid long COVID is to avoid COVID-19 in the first place.
The priority must be to vaccinate vulnerable populations, the elderly, people with underlying medical conditions, and the immunocompromised.
We should ensure at least 70% vaccine coverage for these groups, including both primary and additional booster doses.
...
Announcement
Collapse
No announcement yet.
Discussion - Long COVID
Collapse
X
-
I've heard a lot about LDN being a popular off label treatment.
 Official answer: What is low dose naltrexone? Low dose naltrexone (LDN) means taking a dose of naltrexone that is up to one-tenth, or...
Official answer: What is low dose naltrexone? Low dose naltrexone (LDN) means taking a dose of naltrexone that is up to one-tenth, or...
Low dose naltrexone uses
Low dose naltrexone has been used to treat:
Autoimmune thyroid disorders
Cancer
Chronic fatigue syndrome
Chronic pain
Crohn’s disease
Fibromyalgia
Gulf War syndrome
Multiple sclerosis
Myalgic encephalomyelitis.
-
Full text is available.
Schloss, J.V. Nutritional deficiencies that may predispose to long COVID.
Inflammopharmacol 31, 573–583 (2023). https://doi.org/10.1007/s10787-023-01183-3 Summary
Nutritional deficiencies predispose individuals to severe infection by SARS-CoV-2. COVID-19 disease further exacerbates dietary deficiencies. Stress before or after illness also lowers the stores of essential nutrients. Although zinc (33%) and selenium (14%) are prevalent deficiencies, there are more than 22 different nutritional factors (MND) reported to influence infection outcomes. People at higher risk of infection due to MND are also more likely to have long-term sequelae (Long COVID).
Leave a comment:
-
‘Game changer’: 5 long COVID treatments researchers are most excited about
Gabe Castro-Root
June 15, 2023
snip
Here are five they highlighted.
Low-dose naltrexone
Naltrexone, known more commonly by its brand names Vivitrol and Revia, is a drug made to treat abuse of drugs and alcohol by reducing their effects on the brain. At a low dose, it has shown promise as a treatment for the chronic fatigue that so many long COVID patients experience, according to Dr. Carla Kuon, the co-director of UCSF’s post-COVID clinic.
The drug works by reducing inflammation in the nervous system caused by COVID infection, Kuon said. It does so by regulating the activity of glial cells, which help maintain neurons but can cause inflammation when they’re activated.
“Low-dose naltrexone also has general anti-inflammation effects on the body, and we know inflammation is a big driver of the symptoms of long COVID,” Kuon said. “I personally, as a clinician, have used naltrexone in many patients with success.”
Dr. Hector Bonilla, the co-director of Stanford University’s long COVID clinic, said he also has observed positive results from naltrexone treatment among his patients. But he cautioned that because naltrexone is available as a cheap generic drug, there’s less financial incentive for pharmaceutical companies to fund research into its use as a long COVID treatment. Those trials will be needed to establish its benefits more clearly, he said.
Ivabradine and beta blockers
Ivabradine and beta blockers are different drugs that regulate the heartbeat, slowing it to allow more blood to be pumped with each contraction. These medications are being studied as a treatment for long COVID patients who develop postural orthostatic tachycardia syndrome, or POTS, a condition that results in dizziness and a very fast heartbeat when a person stands.
Ivabradine “has been a game changer” for long COVID patients with POTS, Kuon said.
Hannah Davis, co-founder of the Patient-Led Research Collaborative, a group of researchers who are also long COVID patients, said medications like these are helpful but can be a drain on the body’s resources, often leading to exhaustion when they wear off. She described using a beta blocker as taking energy from the future to support activity in the present.
“If I really have to be present for something, I’ll take a beta blocker knowing I’ll crash later,” Davis said.
A spokesman for Amgen, which manufactures ivabradine, said the company was not actively pursuing long COVID studies with the drug.
Metformin
A recent study from the University of Minnesota found that the anti-diabetic drug metformin reduced the risk of developing prolonged illness by up to 63% for those who started taking it within three days of contracting COVID.
The study, which included over 1,000 participants between ages 30 and 85, suggests the cheap, generic blood sugar medication may prevent viruses from replicating. Its low cost and wide availability could make it an attractive option for preventing long COVID if future research backs up the findings.
Metformin’s “use as a preventive measure could have significant public health implications,” said Dr. Carolyn Bramante, who led the study, in a statement after the results were published.
But the study examined metformin’s use only in preventing long COVID. More research is needed to determine whether the drug is a viable treatment for those already suffering from long COVID.
Antihistamines
COVID frequently causes activation of mast cells, a type of white blood cell found throughout the body. Mast cells release histamines and can lead to allergy-like symptoms including hives, flushing and dizziness. In long COVID patients, those symptoms can drag on long after the initial infection has run its course.
Histamines are also involved in POTS and neuroinflammation, Kuon said, so treating mast cell activation could help reduce other symptoms, too.
Davis said she wants to see clinical trials of prescription antihistamines, but was hopeful over-the-counter ones like benadryl would also prove useful.
A case report published last year in the Journal for Nurse Practitioners showed promise for antihistamine treatments in two long COVID patients, and larger clinical trials are underway.
“I’ll be very interested in those trials because treating mast cell activation is a big part of how I treat long COVID,” Kuon said.
Anticoagulants
Small blood clots are a less common symptom of long COVID, but they can cause low blood-oxygen levels. Patient advocates are pushing for more trials of anticoagulants, which slow or prevent clotting.
“You feel woozy all the time,” Davis said of oxygen deprivation from microclots.
Bonilla said the clots could make full recovery more difficult, since decreased oxygen flow to vital organs means the body’s other functions may not operate at full capacity.
A study published last year in the journal Frontiers in Cardiovascular Medicine found that the drug sulodexide, which treats clotting, significantly improved cardiovascular function and reduced chest pain in long COVID patients. But, as with all potential long COVID treatments, more research is needed to better understand the role of anticoagulants in treating the disease.
more...
Leave a comment:
-
"I know I'm one of the lucky ones- I was boostered when I got my infection and was prescribed Paxlovid - all of which reduce risk (and perhaps improve the course?)."
Maybe or maybe she would have been better off unboosted using treatments other than Paxlovid.
-

Dr. Deepti Gurdasani
@dgurdasani1
Update on what I'm going to now call long COVID symptoms- as it's been 3.5 months since my infection - so am well past the acute stage now. For those who've been following- I've been struggling with breathlessness, chest pain and brain fog post-COVID
8:50 AM · Jun 1, 2023
·
47.2K
Views
241
Retweets
16
Quotes
1,046
Likes
130
Bookmarks
Tweet your reply!
Reply
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
What I've found really debilitating over the past few months is intermittent breathlessness - which occurs on walking, climbing steps, and sometimes just standing up, or walking around the house. It's often accompanied by palpitations (can feel my heart racing), and chest pain.
6
32
347
6,035
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
The symptoms started ~2 wks or so after my acute infection once I started getting out and about and realised that I was getting breathless just on dropping my daughter to school (a twelve minute walk on a very gentle upward slope).
1
21
265
5,380
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
I hadn't even noticed the slope before- but I notice even the most gentle slopes now. I also noticed difficulty with multi-tasking, concentration & memory during this period, but I didn't focus on it much at first because the breathlessness felt far more debilitating and obvious.
2
22
268
5,308
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
But I noticed that I would miss appointments/essential tasks unless I put in a lot more effort- e.g. setting daily alarms & reminders in my calendar for routine task (e.g. school pick ups). I also had difficulty remembering simple things (whether I'd taken my medication).
1
22
262
5,294
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
I don't think it showed as much at work- but I realised the cost of maintaining concentration at meetings was much higher and high often had cognitive equivalent of post-exertion malaise- being exhausted after a day of meetings even if I'd just been sitting at my desk all day.
1
24
249
4,981
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
I had the privilege of being seen by an amazing GP, and consultant, both of whom are very keyed in with long COVID and took my symptoms seriously. I was evaluated for myocarditis, lung clots, and new-onset asthma.
1
24
251
4,611
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
My echocardiogram (test for heart function), cardiac enzymes (test for heart muscle inflammation) were normal. My ventilation-perfusion scan showed slight abnormalities but nothing specific that suggested large clots (cannot rule out microclots with this).
1
19
224
4,508
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
Lung functions (that look for things like new-onset asthma) were also normal. At about 6 weeks or so, I started seeing a regular improvement in symptoms. The improvement wasn't monotonic (as in every day better than the last), but more in the form of fewer bad days than before.
1
16
217
4,278
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
But there was a lot of fluctuation day to day, and it was hard to get a handle on where I'd gotten to in terms of improvement. But slowly I found I was able to walk to school, and on some days even brisk walk without getting breathless. One day I was even able to run with breaks.
1
14
210
4,112
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
My brain fog also improved a lot, and I was able to manage a bigger cognitive load- and do a lot more multi-tasking mentally. It didn't improve to baseline, but in terms of function, I was doing much better, although still at a higher cost of functioning (exhausted afterwards).
1
14
210
4,093
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
Then, oddly about two weeks ago, things took a turn for the worse. I cannot pin-point to anything that necessarily triggered it- but there were days I was breathless just getting out of bed or trying to fix lunch. And needing to stop 2-3 times just walking slowly to school.
4
17
225
4,071
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
The breathlessness and tachycardia has been more frequent- daily for the last week. I don't know what changed this, because I felt I was on a trajectory where things were definitely getting better. I don't know for sure, but I have identified some triggers.
1
15
208
4,075
Dr. Deepti Gurdasani
@dgurdasani1
·
2h
I've noticed that lack of sleep, longer gaps between meals, and heated blankets/hot showers, coffee tend to make it worse. This is what makes me think it's POTS-related - as the breathlessness is accompanied by a high heart rate, but my sats are in the normal range.

Dr. Deepti Gurdasani
@dgurdasani1
·
3h
I'm not entirely sure what the next steps are- am planning to see a POTS specialist, but wanted to share this - in case there are others who have been hit with very fluctuating symptoms - with promising early improvement followed by worsening - rather than a clear trajectory.
6
19
291
5,338
Dr. Deepti Gurdasani
@dgurdasani1
·
3h
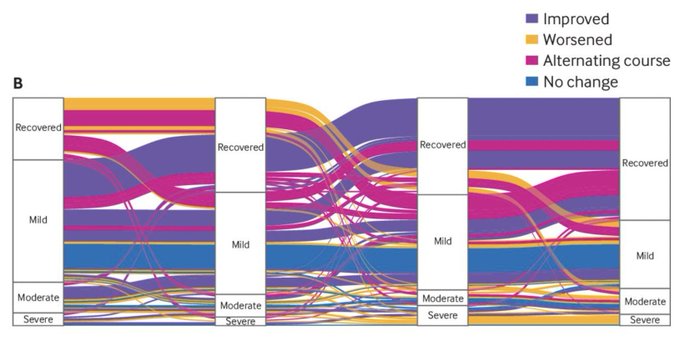
This recent paper from the BMJ shows that a significant proportion of people have a sort of relapsing-remitting course - moving between recovery and symptoms, or different severity categories. So, I guess it isn't unusual. https://bmj.com/content/381/bmj-2022-074425…
1
46
297
6,209
Dr. Deepti Gurdasani
@dgurdasani1
·
3h
Still hoping that this will gradually improve over time, although will moderate my expectations better, as the worsening after the early improvement did take me by surprise, and was quite disheartening.
2
17
251
4,752
Dr. Deepti Gurdasani
@dgurdasani1
·
3h
I know I'm one of the lucky ones- I was boostered when I got my infection and was prescribed Paxlovid - all of which reduce risk (and perhaps improve the course?). Unlike many others, I also have the luxury of being able to work from home, and limit my activity.
2
16
257
4,803
Dr. Deepti Gurdasani
@dgurdasani1
·
3h
It does affect me significantly day to day, and has been really debilitating - and I know my symptoms are probably far less severe than many others. I can't imagine having to live with this for years on end - as I know many have been.
2
21
260
4,762
Dr. Deepti Gurdasani
@dgurdasani1
Many people made gaslit me & trolled me when I said I was very wary about getting infected because of the risk of long COVID. I have ulcerative colitis, and the few studies done on this and COVID show that the risk of long COVID is between 50-70% for someone with my risk profile
8:51 AM · Jun 1, 2023
·
8,414
Views
Leave a comment:
-
OPINION
As long COVID turns three, Americans play disability roulette
As an ICU physician, I’ve had a front-row seat to the heartbreak of the past three years.
By Wes Ely
Updated May 26, 2023, 3:00 a.m.
snip
The Department of Health and Human Services considers long COVID a disability. Yet these patients fall through the cracks. They are often let down by physicians who are unclear how to diagnose an illness so new and varied. They are repeatedly denied disability benefits and struggle to find health care because they are newly out of work and without insurance. A recent National Institutes of Health-sponsored study at 44 US medical centers found 56 percent of people hospitalized with COVID-19 struggled to pay their bills six months out due to ongoing heart and lung problems. Even bathing and preparing meals is hard for many.
Take Trinity Peacock. A 20-year-old student from Atlanta, she spoke to me in my office about how a super-spreader family funeral in 2021 left several of her loved ones with long COVID. “My family has been offered no support in any way. No therapy, no compensation,” she told me. “The COVID convo has died down while we are left to suffer.” It’s been two years, and multiple people in her family have ongoing problems with long COVID.
Numerous studies document the haunting brain impacts of long COVID, from loss of supportive cells in the brain called glial cells, to early death of our neurons leading to signs of early dementia in too many long COVID patients, even young ones who had only mild infectious symptoms during their initial COVID infection. Among the 10 percent of patients estimated to get long COVID, many of them experience cardiac problems like a racing heart and profound dizziness when they try to stand or sleep. Some have cramps, diarrhea, and bloating owing to problems with shifts in gut bacteria in antibiotic-treated COVID patients referred to as “gut dysbiosis,” which means that the normal bacteria are replaced with more dangerous blooms of organisms that wreak havoc on overall health by enabling dangerous secondary infections during and after COVID.
more.... https://www.bostonglobe.com/2023/05/...lity-roulette/
Leave a comment:
-
So obesity and prior drinking history are risks. Go figure.
 Medical experts are seeing a suspected link between post-COVID effects and people developing alcohol intolerance.
Medical experts are seeing a suspected link between post-COVID effects and people developing alcohol intolerance.
Long COVID may make your hangovers much worse, researchers say
By Adriana Diaz
January 20, 2023 6:59pm
Getting a positive COVID-19 test may not only affect the way people taste and smell alcohol — it may also change the way they process it.
Anecdotal data has found that some people have reported a change in how their bodies react to booze after testing positive for the coronavirus.
Rebekah Stein, 30, used to be able to hold her liquor before being diagnosed with COVID in March 2020, she told BuzzFeed News.
Then one night after her mild symptoms went away, she casually stole a sip of her husband’s whiskey, as she had done plenty of times before...
Leave a comment:
-
https://onlinelibrary.wiley.com/doi/...002/acn3.51631
Tziastoudi, M., Cholevas, C., Stefanidis, I. and Theoharides, T.C. (2022), Genetics of COVID-19 and myalgic encephalomyelitis/chronic fatigue syndrome: a systematic review. Ann Clin Transl Neurol, 9: 1838-1857. https://doi.org/10.1002/acn3.51631
Abstract
COVID-19 and ME/CFS present with some similar symptoms, especially physical and mental fatigue. In order to understand the basis of these similarities and the possibility of underlying common genetic components, we performed a systematic review of all published genetic association and cohort studies regarding COVID-19 and ME/CFS and extracted the genes along with the genetic variants investigated. We then performed gene ontology and pathway analysis of those genes that gave significant results in the individual studies to yield functional annotations of the studied genes using protein analysis through evolutionary relationships (PANTHER) VERSION 17.0 software. Finally, we identified the common genetic components of these two conditions. Seventy-one studies for COVID-19 and 26 studies for ME/CFS were included in the systematic review in which the expression of 97 genes for COVID-19 and 429 genes for ME/CFS were significantly affected. We found that ACE, HLA-A, HLA-C, HLA-DQA1, HLA-DRB1, and TYK2 are the common genes that gave significant results. The findings of the pathway analysis highlight the contribution of inflammation mediated by chemokine and cytokine signaling pathways, and the T cell activation and Toll receptor signaling pathways. Protein class analysis revealed the contribution of defense/immunity proteins, as well as protein-modifying enzymes. Our results suggest that the pathogenesis of both syndromes could involve some immune dysfunction.
Leave a comment:
-
9 at-home exercises that may help relieve your long COVID symptoms
BY Barbara Brody
November 29, 2022, 6:00 PM UTC
Leave a comment:
-

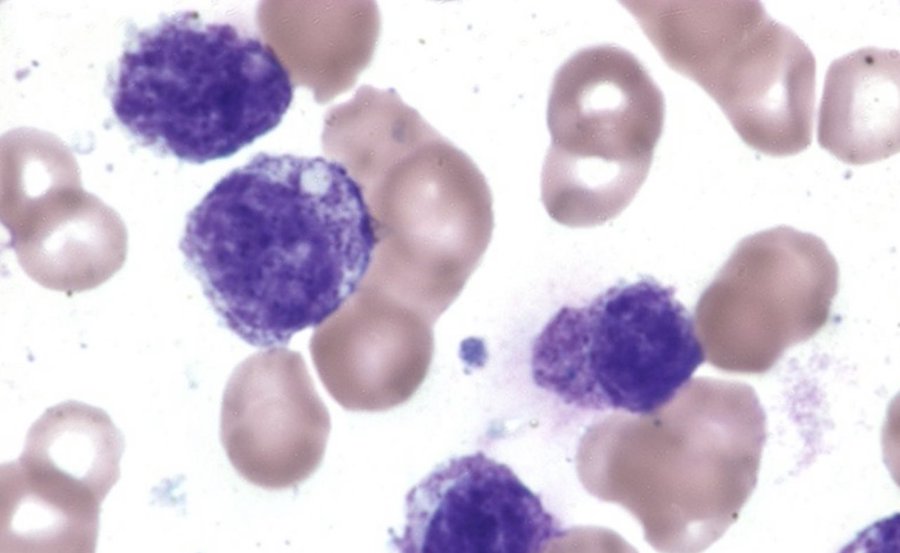
Dr Claire Taylor
@drclairetaylor
1/ Mast Cell Monday. What are ‘mast cells’? They are part of the immune system and constantly looking for trouble! Handy wee things when you need them- they release histamine+ other things to draw other cells to the area. The problem is when they go rogue…
10:20 AM · Nov 14, 2022·Twitter for iPhone
618
Retweets
85
Quote Tweets
2,158
Likes

Tweet your reply
Reply
Dr Claire Taylor
@drclairetaylor
·
22h
Replying to
@drclairetaylor
2/ they can go rogue for no reason and this is called ‘mast cell activation syndrome’ Eg the mast cells are acting like there is a big problem and releasing all these chemicals eg Histamine and prostaglandins that can then cause symptoms in every part of the body.
10
37
473
Dr Claire Taylor
@drclairetaylor
·
22h
5/ the list of symptoms is endless but commonly fast heart rate, rashes, reflux, headaches, fatigue, gastro symptoms. Triggers can be food, temperature, smells, chemicals, exercise, stress or nothing at all. At worst can lead to anaphylaxis (should stress this is rarer).
8
53
477
Dr Claire Taylor
@drclairetaylor
·
22h
6/ how common is it? According to one dr up to 17% of the population. Answer is we don’t really know but it’s associated with #mecfs #LongCovid and other immune medicated diseases
5
26
409
Dr Claire Taylor
@drclairetaylor
·
22h
7/ why hasn’t your Doctor heard of it? It appears in the ICD-10 coding of diseases https://aapc.com/codes/icd-10-codes/D89.4… Yet there are no guidelines and not a huge amount of research. There is an international consensus statement
pubmed.ncbi.nlm.nih.gov
Diagnosis of mast cell activation syndrome: a global "consensus-2" - PubMed
The concept that disease rooted principally in chronic aberrant constitutive and reactive activation of mast cells (MCs), without the gross MC neoplasia in mastocytosis, first emerged in the 1980s,...
2
50
433
Dr Claire Taylor
@drclairetaylor
·
22h
8/ Are there tests? Yes. But any mcas patient will tell you that they are often negative - blood tryptase level -24 urine tests that have to be kept on ICE and degrade quickly.
3
17
346
Dr Claire Taylor
@drclairetaylor
·
22h
9/ is there treatment? Yes! Which is why we need to raise awareness of it as a condition. We have seen a huge increase in #mcas after Covid.
@BethanMyers
has written the best paper on it. I bow to her expertise.
pubmed.ncbi.nlm.nih.gov
Mast cell activation syndrome and the link with long COVID - PubMed
Mast cells are innate immune cells found in connective tissues throughout the body, most prevalent at tissue-environment interfaces. They possess multiple cell-surface receptors which react to...
8
86
506

Dr Claire Taylor
@drclairetaylor
·
22h
10/ treatment can start with most basic H1 and H2 blockers ( eg antihistamines and H2 blockers formerly used mainly for stomach problems). There are then various groups of meds that can be worked up to if things are not settling.
10
30
343
Dr Claire Taylor
@drclairetaylor
·
22h
11/ this study showed that Long-COVID patients had similar severity of numerous MCAS symptoms
ijidonline.com
Mast cell activation symptoms are prevalent in Long-COVID
The COVID-19 pandemic has spread throughout the world, with calamitous outcomes for some of those acutely infected and for those who struggle with Long-COVID (LC), also known as Long-Haul COVID and...
2
54
325
Dr Claire Taylor
@drclairetaylor
·
22h
12/ children also get it. This paper from 2020 questions whether multisystem inflammation is actually severe MCAS https://mastcellaction.org/assets/2021/09/17/53330e05-1552-4b3b-9238-25a39a80ec0b.pdf?v=1…
@LongCovidKids
1
21
272
Dr Claire Taylor
@drclairetaylor
·
22h
13/ is irritable bowel syndrome actually MCAS? This study showed IBS patients had increased mast cells near the nerves.
sciencedirect.com
Activated mast cells in proximity to colonic nerves correlate with abdominal pain in irritable...
Background & Aims: The mechanisms underlying abdominal pain perception in irritable bowel syndrome (IBS) are poorly understood. Intestinal mast cell i…
4
49
383
Dr Claire Taylor
@drclairetaylor
·
22h
14/ MCAS is associated with #MECFS #LongCovid #EhlersDanlos #pots It’s hard to get numbers on how many are affected but from clinical observation it appears to be a lot. So we have a treatable avenue but patients have to actively seek out diagnosis and treatment
4
26
337
Dr Claire Taylor
@drclairetaylor
·
22h
16/ MCAS is different from mastocytosis. In MCAS there are normal cells that rerelease chemicals when they shouldn’t. Mastocytosis is when the body makes too many mast cells.
4
19
282
Dr Claire Taylor
@drclairetaylor
·
22h
17/ I hope this is helpful for patients and #MedTwitter Picture of mast cell ( from https://marekdoyle.com/mast-cell-activation-messenger/…) #NEISvoid
15
20
310
Dr Claire Taylor
@drclairetaylor
21h
Haven’t a clue where tweets 3+4 went. That’s what happens when you tweet and parent at the same time
Leave a comment:
-
You can skip the intro and go to 22:35 "Questions we will explore about long-haul covid" if you want.
Long-haul Covid symptoms and Cervical Instability overlap and Vagus Nerve Connection
Caring Medical
98.7K subscribers
401,307 views May 7, 2022
In this nearly 2 hour webinar, Ross Hauser, MD reviews some medical articles on long covid and discusses the overlap of symptoms in patients diagnosed with long covid and those who have cervical instability and vagus nerve degeneration. He begins by sharing a very personal statement and update on Caring Medical Florida.
Leave a comment:
-
https://onlinelibrary.wiley.com/doi/...002/jcsm.12931
Sarcopenia as potential biological substrate of long COVID-19 syndrome: prevalence, clinical features, and risk factors
Martone, A. M., Tosato, M., Ciciarello, F., Galluzzo, V., Zazzara, M. B., Pais, C., Savera, G., Calvani, R., Marzetti, E., Robles, M. C., Ramirez, M., Landi, F., and Gemelli Against COVID-19 Post-Acute Care Team (2022) Sarcopenia as potential biological substrate of long COVID-19 syndrome: prevalence, clinical features, and risk factors, Journal of Cachexia, Sarcopenia and Muscle, 13, 1974– 1982, https://doi.org/10.1002/jcsm.12931
Conclusions
Sarcopenia identified according to the EWGSOP2 criteria is high in patients recovered from COVID-19 acute illness, particularly in those who had experienced the worst clinical picture reporting the persistence of fatigue and dyspnoea. Our data suggest that sarcopenia, through the persistence of inflammation, could be the biological substrate of long COVID-19 syndrome. Physical activity, especially if associated with adequate nutrition, seems to be an important protective factor.
Leave a comment:
-
Dana Parish
@danaparish
·
18h
People are often asking what blood tests they can request to look for Covid vascular damage/ microclotting issues
Quote Tweet

Resia Pretorius
@resiapretorius
·
Oct 29
We have shown that molecules secreted by damaged endothelia may be used in interim ‘til we have microclot lab tests.Try pathlabs for VWF, e-selectin and PECAM-1, ALSO alpha2antiplasmin. Most trapped in clots - so soluble fraction = not total concentration @dbkell @doctorasadkhan twitter.com/Sunny_Rae1/sta…
Leave a comment:
-
hat tip to @ann_mcnitt for link
Dr Claire Taylor

2h • 17 tweets • 5 min read Bookmark Save as PDF My Authors
Clinical pearls for #LongCovid
1. Find the clots. They are there. If not PE or DVT there are Microclots. 100% of all long Covid patients tested so far have them.
2. If you don’t find PE on CTPA, do a VQ or dual energy CT. You will find the missed clots.
3. Test for Autonomic dysfunction (Covid has a predilection for the ANS).
A 10 minute stand test will suffice. batemanhornecenter.org/wp-content/upl…
4. Then treat said autonomic dysfunction. Don’t tell people it’s ok to have a pulse of 160 doing the dishes. Great info at pots.org
5. Assess for mast cell activation syndrome. Some will says it’s not real. It’s real. Check for dermatographism. Ask about alcohol intolerance, new allergies, new rashes, urticaria. Etc etc
6. You don’t need fancy tests. Just treat it and see response. More info at @MastCellAction
7. Don’t tell people exercise will cure it. It won’t. It didn’t cure #MECFS and it won’t cure long Covid.
74% of patients felt worse with exercise in this study
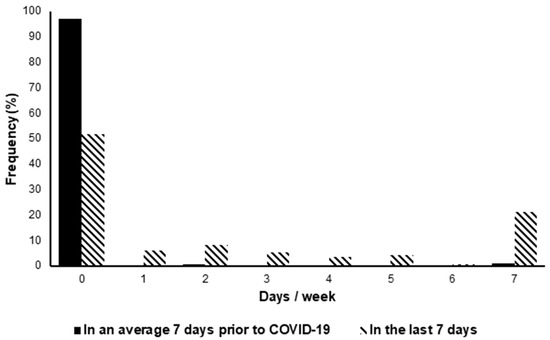
The Relationship between Physical Activity and Long COVID: A Cross-Sectional StudyThe relationship between Long Covid (LC) symptoms and physical activity (PA) levels are unclear. In this cross-sectional study, we examined this association, and the advice that individuals with LC re…https://www.mdpi.com/1660-4601/19/9/...HsvjzuwzCHgcsM
8. Don’t tell people it is psychological. They have been infected with a level 3 biohazard with unknown repercussions.
9. Don’t tell them to think themselves better, to try harder. They are already trying.
10. Advise them on pacing, which is a way of using what energy is available without crashing.
Familiarise yourself with post-exertional malaise- you are you are going to be seeing a LOT of it over the next few years. See @LongCOVIDPhysio
11. Don’t dismiss chest pain. This shouldn’t even have to be said but unfortunately does.
19% of long Covid patients in the coverscan study had myocarditisAlmost 1 in 5. Treat it. It’s not anxiety.

Multiorgan impairment in low-risk individuals with post-COVID-19 syndrome: a prospective, community-based studyObjective To assess medium-term organ impairment in symptomatic individuals following recovery from acute SARS-CoV-2 infection. Design Baseline findings from a prospective, observational cohort study…https://bmjopen.bmj.com/content/11/3/e048391
12. Try not to catch Covid yourself - you have between 1 in 10 and 1 in 20 chance each infection.
Damage is likely to be cumulative. It affects all the organs as every organ has a blood supply.
13. don’t think because you felt ok after one infection that this will be the case after 5 infections. (We can’t get long term immunity to this virus no matter what anyone on Twitter says).
14. Don’t listen to people who say it’s a cold- it’s not. It’s really really not. Colds don’t cause organ dysfunction and blood clots.
15. Anyone who uses this emoji 💉 over and over has an agenda. We knew the damage Covid caused in January 2020, well before the 💉
16. Protect the children from all of the above. They will be the generation with early heart disease. #CovidIsNotOver #MedTwitter #COVIDIsAirborne #CleanAirClassrooms #dontlookup
Leave a comment:








Leave a comment: